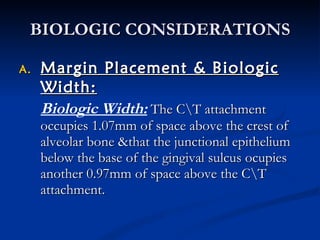
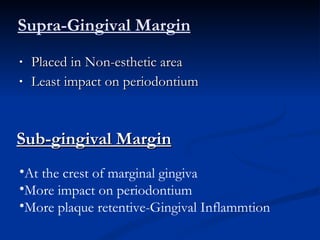
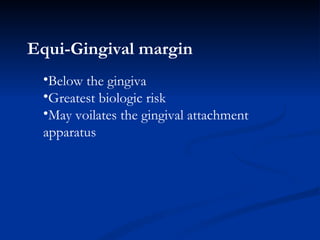
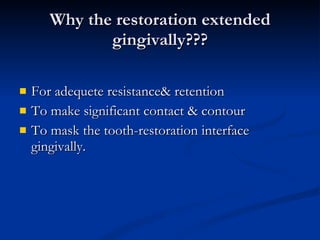
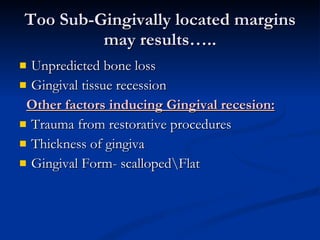
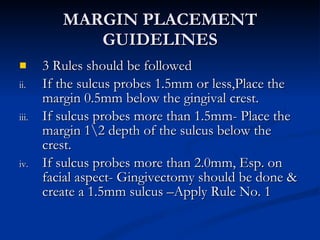
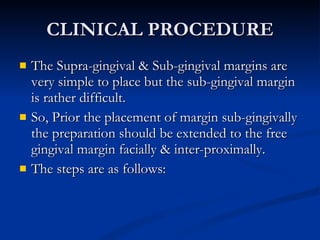
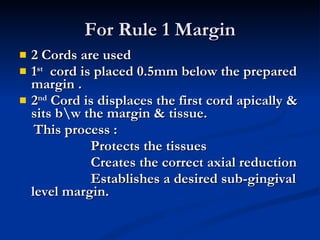
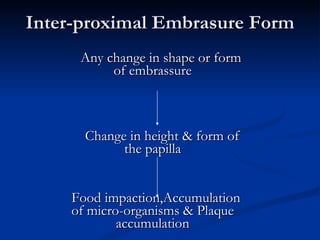
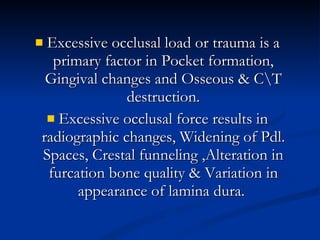
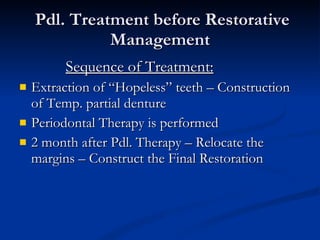
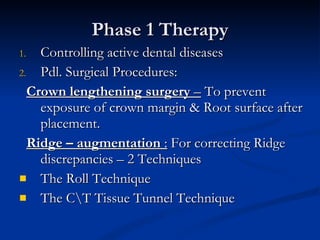
The relationship between periodontal health and dental restorations is intimate and interdependent. Properly placing restoration margins is important to avoid biological width violations and maintain periodontal health. Restoration contours and occlusion also impact the periodontium, and periodontal treatment may be needed before or during restorative procedures to optimize outcomes.