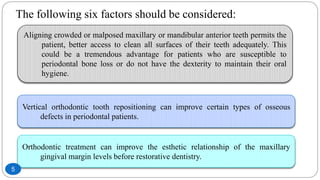
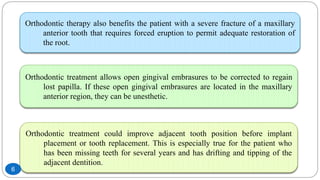
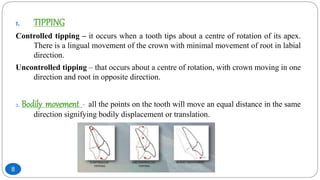
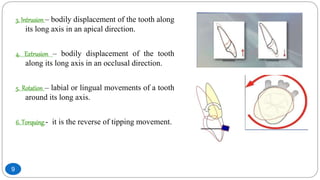
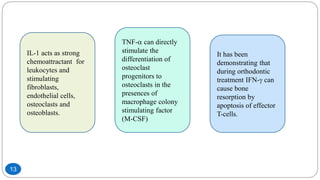
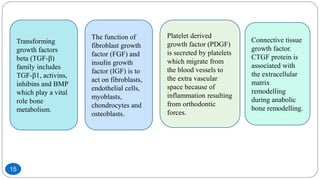
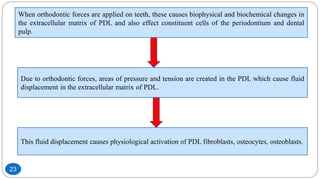
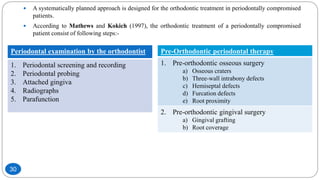
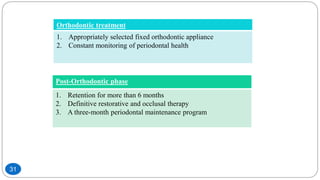
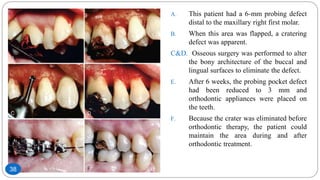
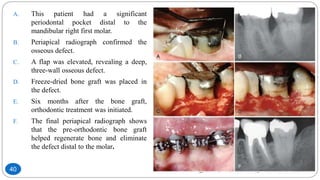
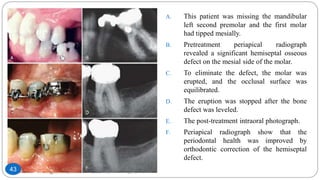
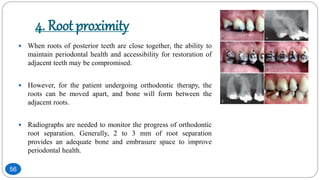
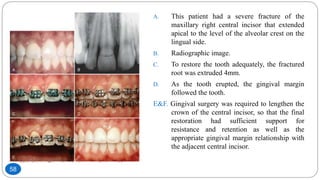
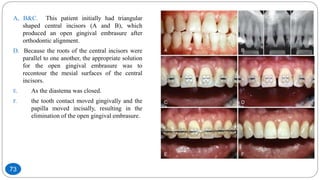
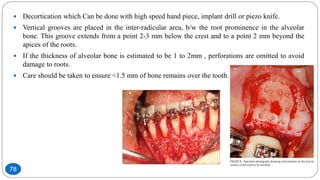
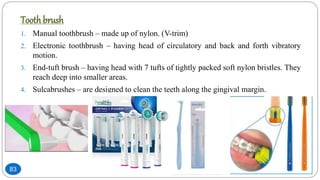
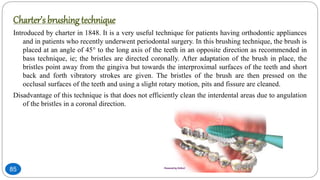
The document discusses the interdisciplinary approach involving orthodontic therapy and periodontal treatment, highlighting the benefits, types of tooth movement, and the biological processes involved in orthodontic tooth movement. It outlines the sequence of orthodontic treatment for periodontally compromised patients, emphasizing the importance of periodontal examination and necessary pre-orthodontic surgeries. Additionally, the document details the roles of molecular and cellular biology in the context of orthodontic forces and their effects on surrounding tissues.