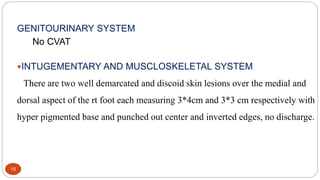
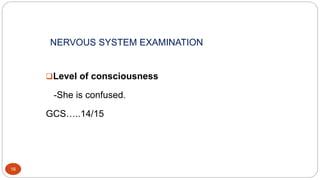
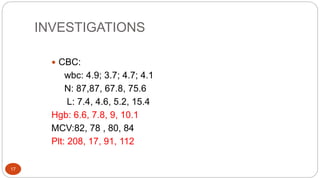
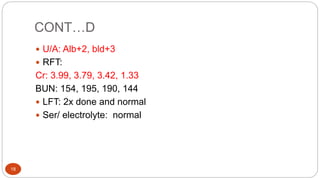
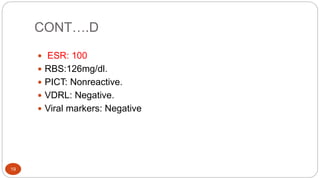
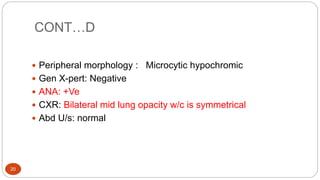
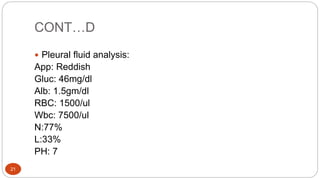
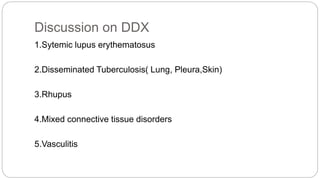
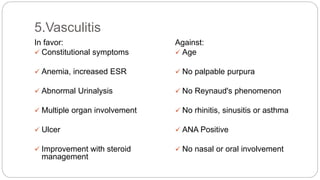
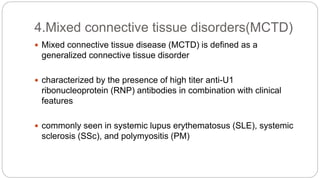
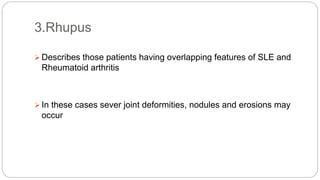
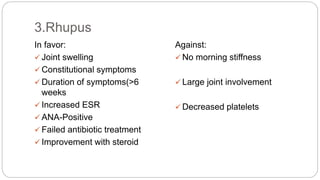
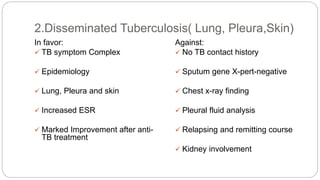
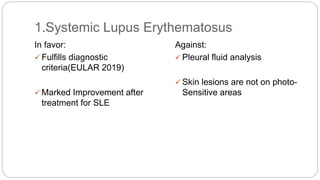
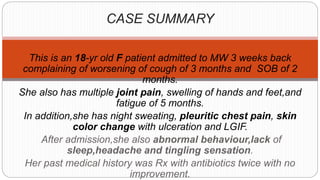
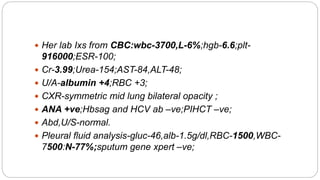
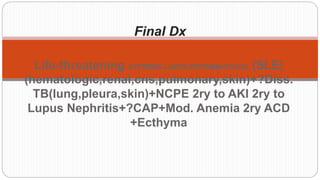
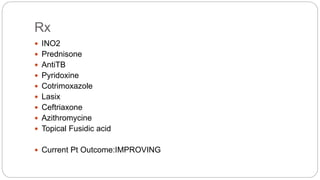
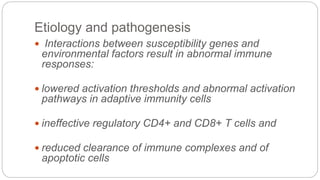
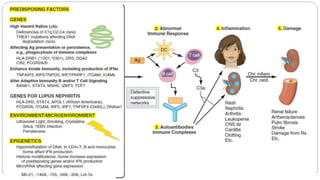
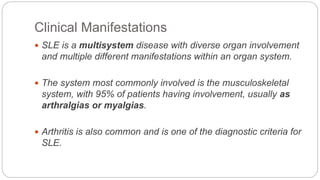
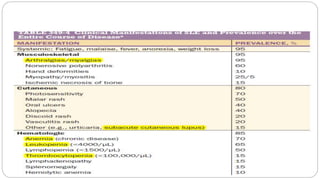
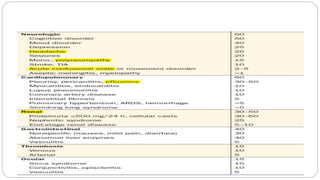
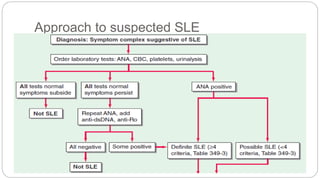
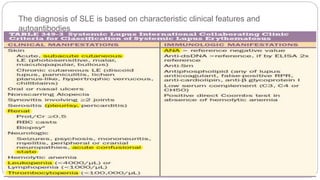
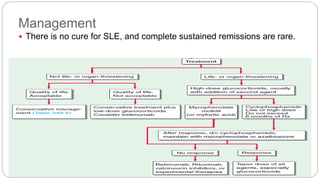
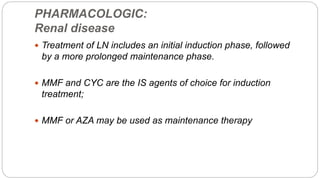
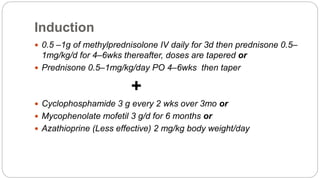
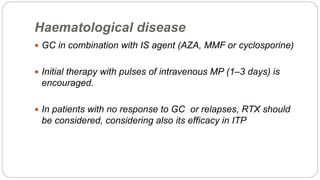
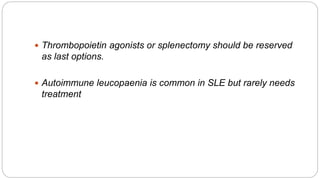
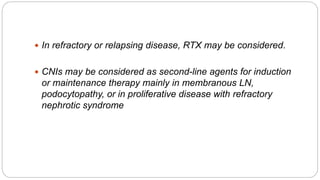
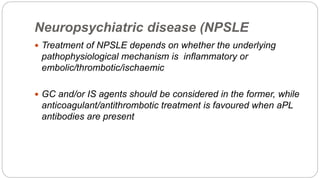
This case discusses an 18-year-old female patient presenting with easy fatigability and other symptoms over several months. After examination and investigations, she was diagnosed with systemic lupus erythematosus affecting multiple organs including the lungs, skin, kidneys, and central nervous system. She was started on treatment including steroids, antibiotics, and other medications. The case highlights the approach to diagnosing and managing SLE, a chronic autoimmune disease with diverse clinical manifestations and organ involvement.