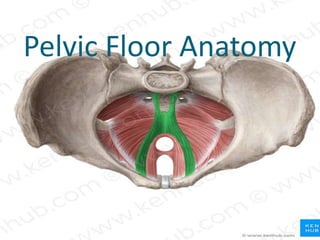
The document provides an extensive overview of pelvic floor anatomy, its functions, and common dysfunctions that affect women, including risk factors, assessment methods, and treatment options. It highlights the importance of pelvic floor muscles in supporting internal organs, maintaining continence, and influencing sexual function, as well as the challenges many women face in seeking help for pelvic floor dysfunction (PFD). Treatment recommendations include lifestyle modifications, dietary adjustments, and specific therapeutic techniques to manage both hypertonicity and hypotonicity of pelvic floor muscles.