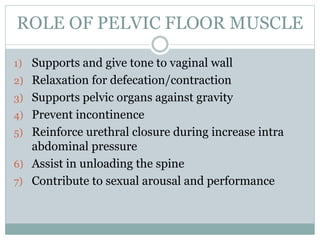
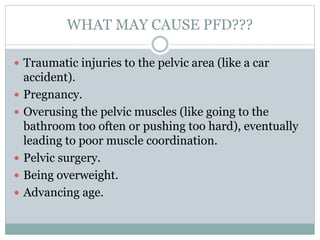
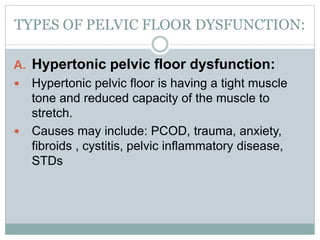
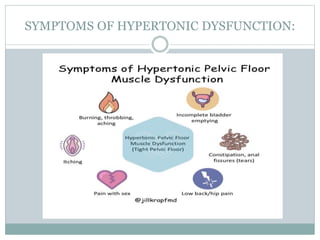
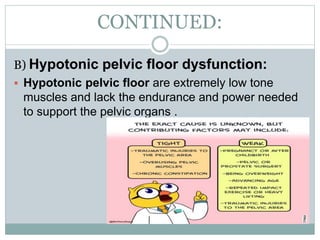
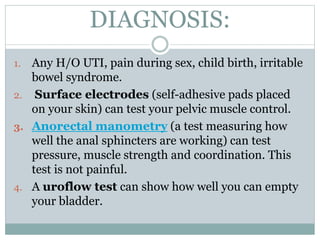
Pelvic floor dysfunction (PFD) is a common issue characterized by the inability to properly relax and coordinate pelvic floor muscles, affecting urination and bowel movements. Causes include traumatic injuries, pregnancy, pelvic surgery, and aging, with symptoms ranging from pain to incontinence. Management through pelvic floor physical therapy (PFPT) involves education, strengthening exercises like Kegels, and various techniques to improve coordination and reduce pain.