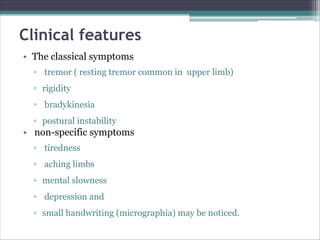
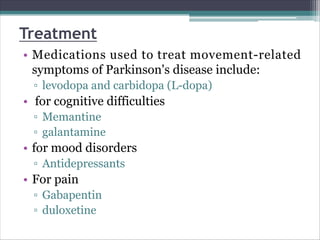
Parkinson's disease is a chronic neurodegenerative disorder characterized by the gradual loss of dopaminergic neurons in the basal ganglia, leading to a range of motor symptoms such as bradykinesia, rigidity, and tremors, along with non-motor symptoms including cognitive decline and mood changes. The disease's etiology remains unclear, but risk factors include genetic predisposition, exposure to toxins, and age, with incidence rates differing globally. Treatment options involve medications, physical therapy, and deep brain stimulation to manage symptoms and improve quality of life.