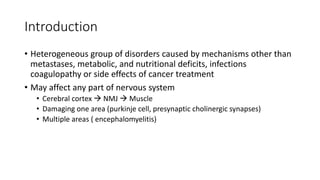
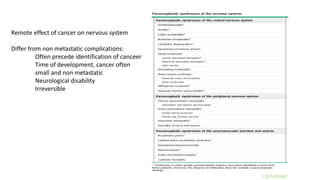
This document discusses neurological paraneoplastic syndrome, a heterogeneous group of neurological disorders caused by an immune response to cancer rather than directly from the cancer or its treatment. Key points:
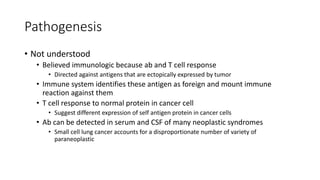
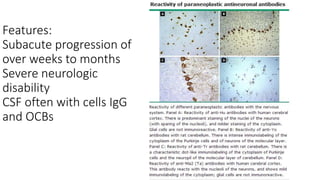
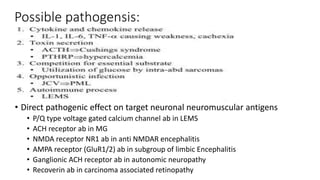
- The immune system mounts an abnormal response against antigens expressed by the cancer that are similar to neuronal antigens, leading to damage of nerve or muscle tissue.
- Symptoms can include problems in the cerebral cortex, neuromuscular junction, or multiple areas of the nervous system. Neurological disability is often severe and irreversible.
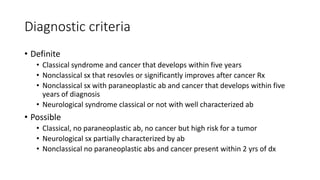
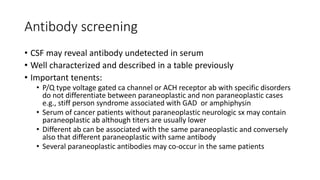
- Diagnosis involves identifying well-characterized antibodies, detecting cancer within 5 years, and ruling out other causes. Screening cancer patients without neurological symptoms still occasionally finds paraneoplastic antibodies.