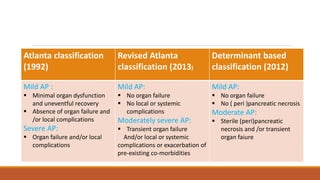
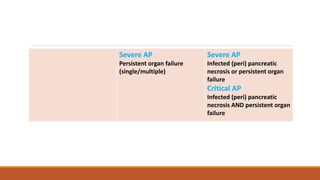
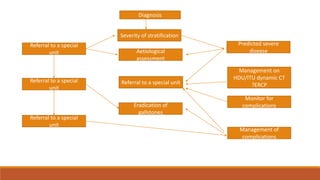
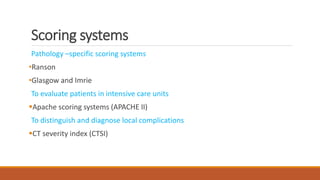
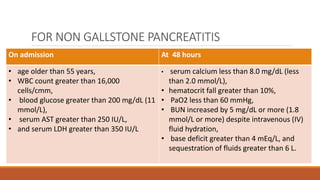
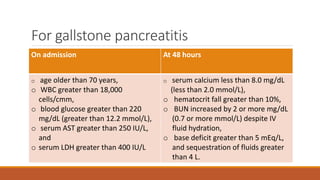
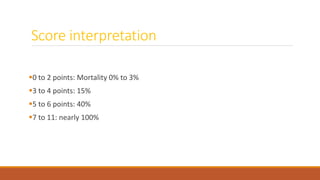
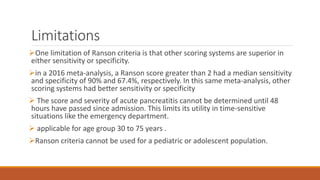
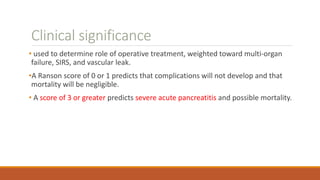
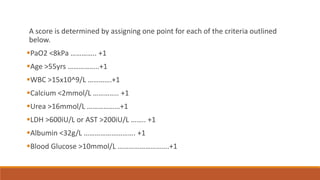
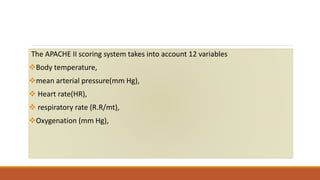
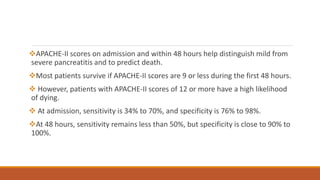
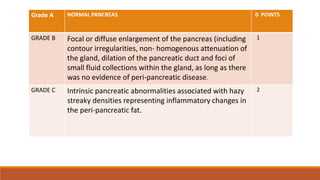
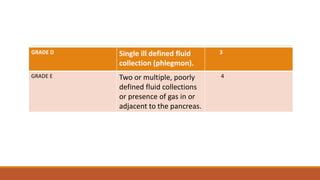
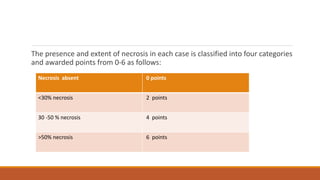
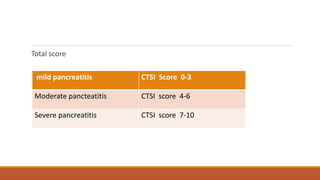
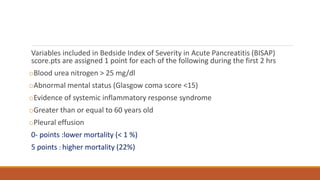
This document discusses several scoring systems used to assess the severity of acute pancreatitis, including the Atlanta classification, revised Atlanta classification, determinant-based classification, Ranson score, Glasgow score, APACHE II score, CT severity index, Marshall score, SOFA score, BISAP score, and harmless acute pancreatitis score. It provides details on the criteria included in each scoring system and how they are used to stratify pancreatitis as mild, moderate, or severe. The limitations and clinical significance of several common scoring systems like Ranson, APACHE II, and CT severity index are also reviewed.