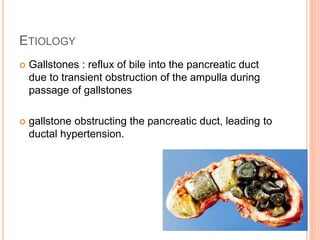
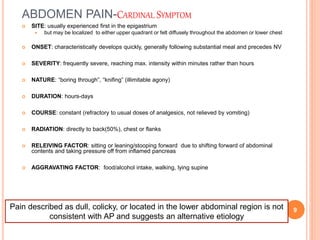
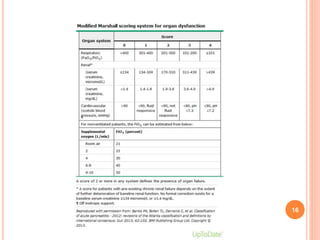
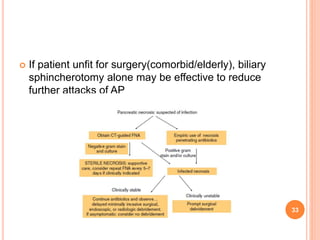
Acute pancreatitis is an inflammatory condition of the pancreas characterized by abdominal pain and elevated pancreatic enzymes. The most common causes are gallstones and alcohol. In severe cases, pancreatic enzymes activate prematurely and digest the pancreas. This can lead to systemic inflammatory response and organ failure. Diagnosis is based on abdominal symptoms and blood tests showing elevated pancreatic enzymes. Severity is assessed using criteria like Marshall score and need for ICU care. Treatment involves hydration, pain control, treating the underlying cause, preventing infection, and nutrition support. Surgery is usually not needed for sterile pancreatic necrosis but may be for infected necrosis after 4 weeks.