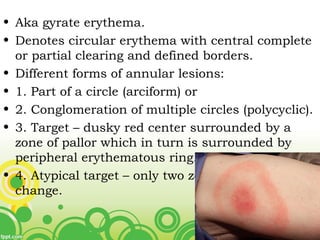
This document describes various types of annular and figurate erythemas. It defines figurate erythemas as circular erythemas with central clearing and defined borders that can take the form of arcs, circles, or targets. It then discusses specific conditions that present as annular erythemas such as erythema annulare centrifugum, erythema migrans, erythema marginatum rheumaticum, and others. For each condition, it outlines their clinical features, etiologies, histology, diagnosis, and treatment. Differential diagnoses are also provided.