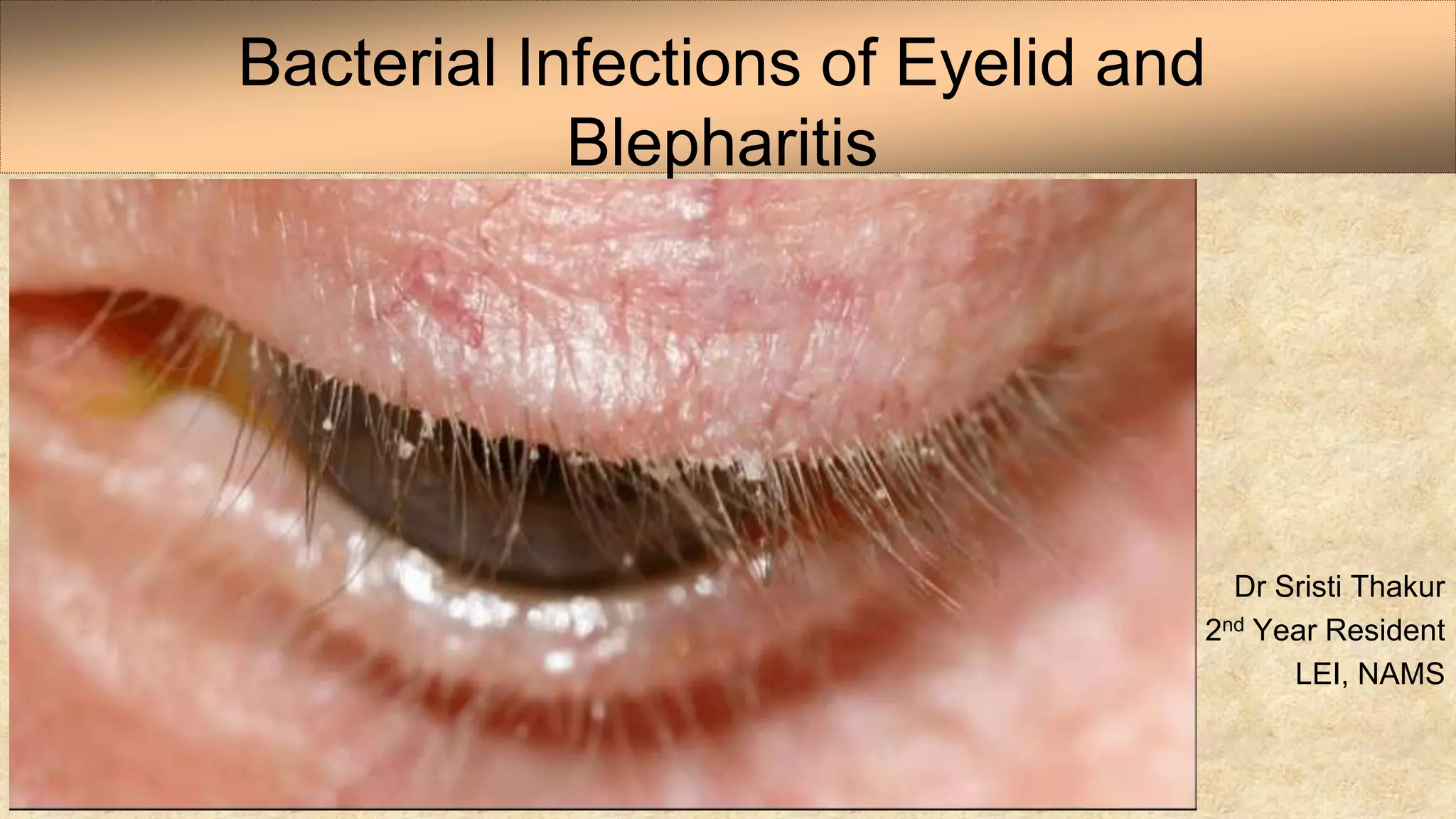
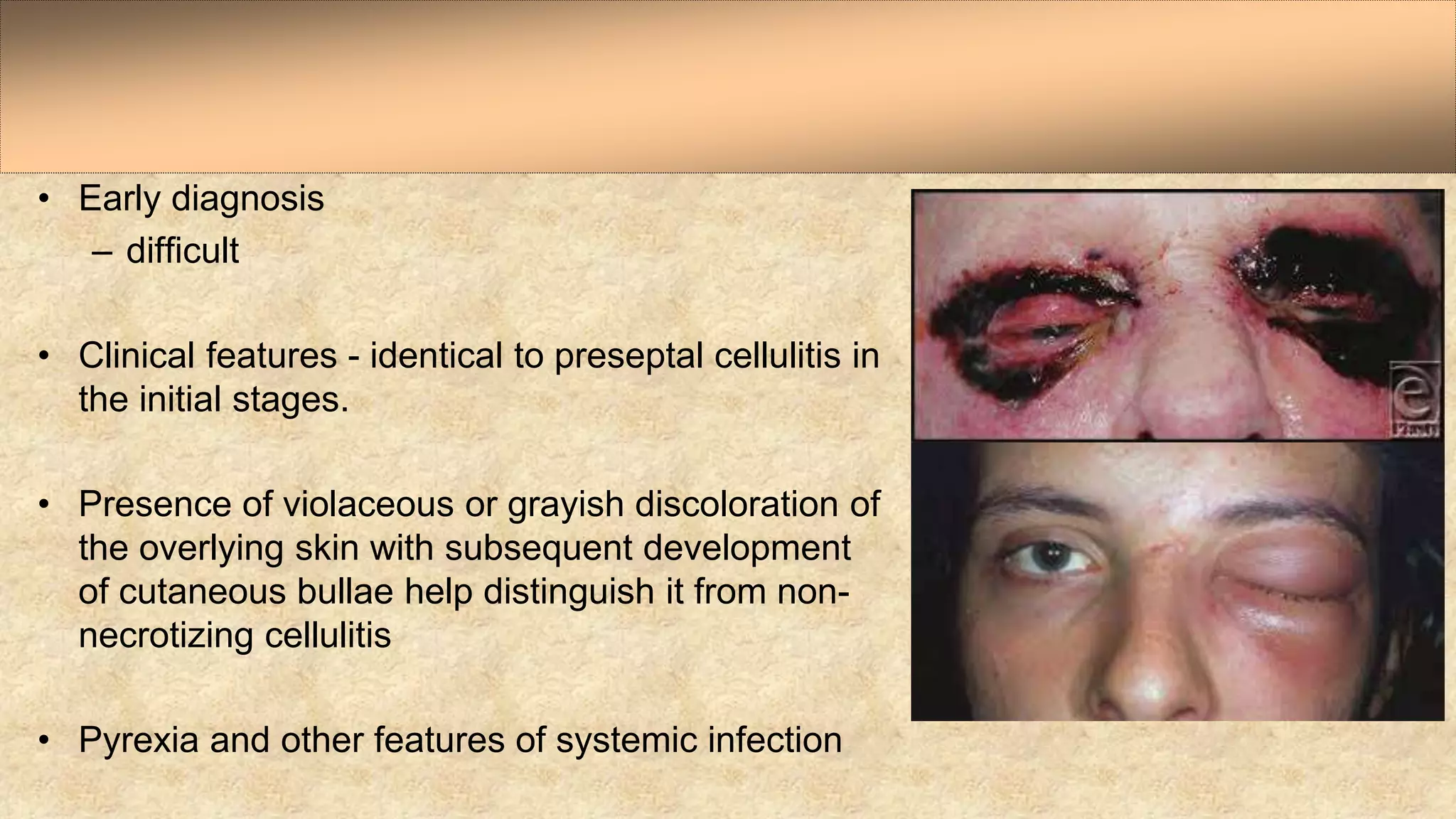
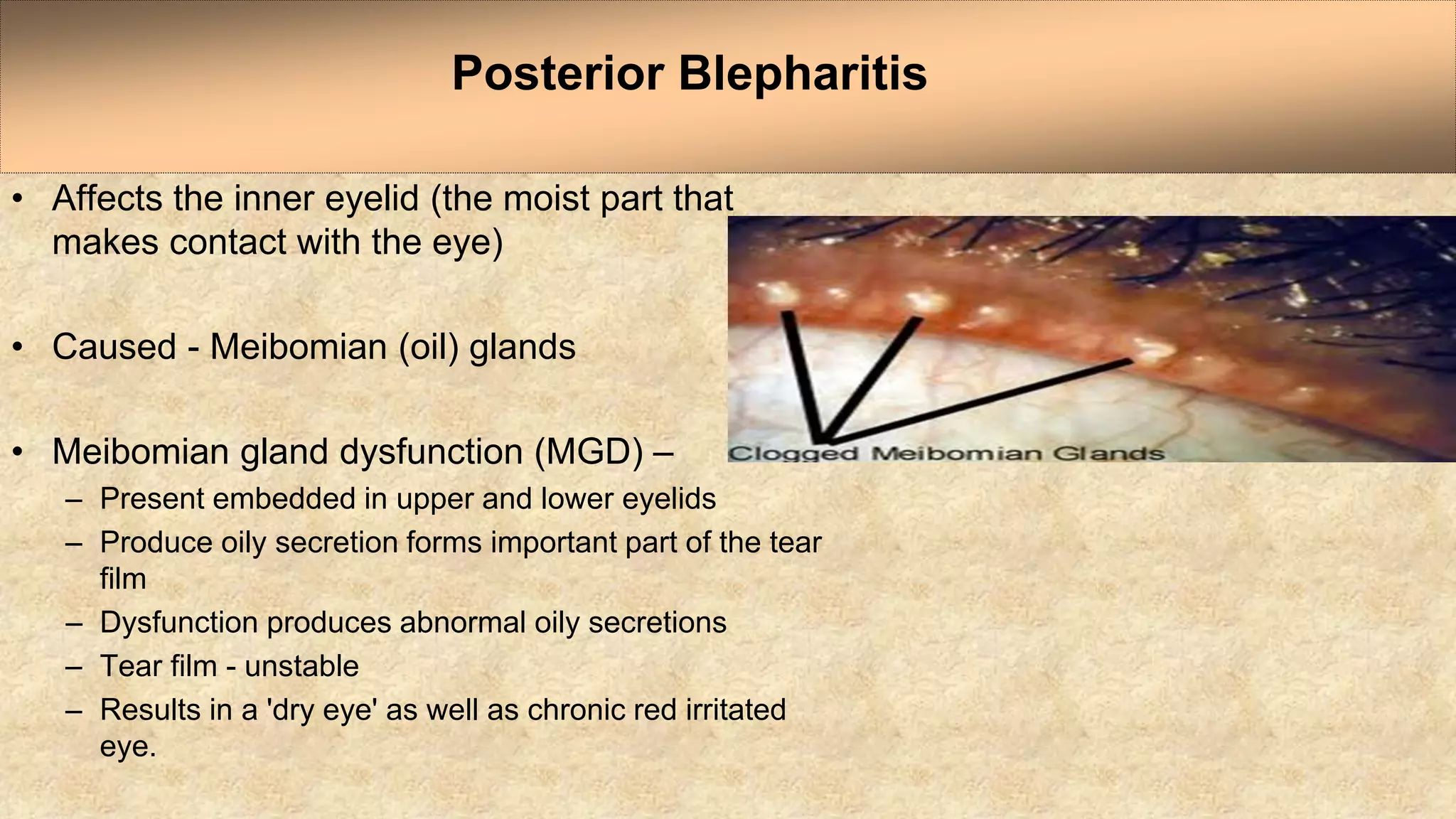
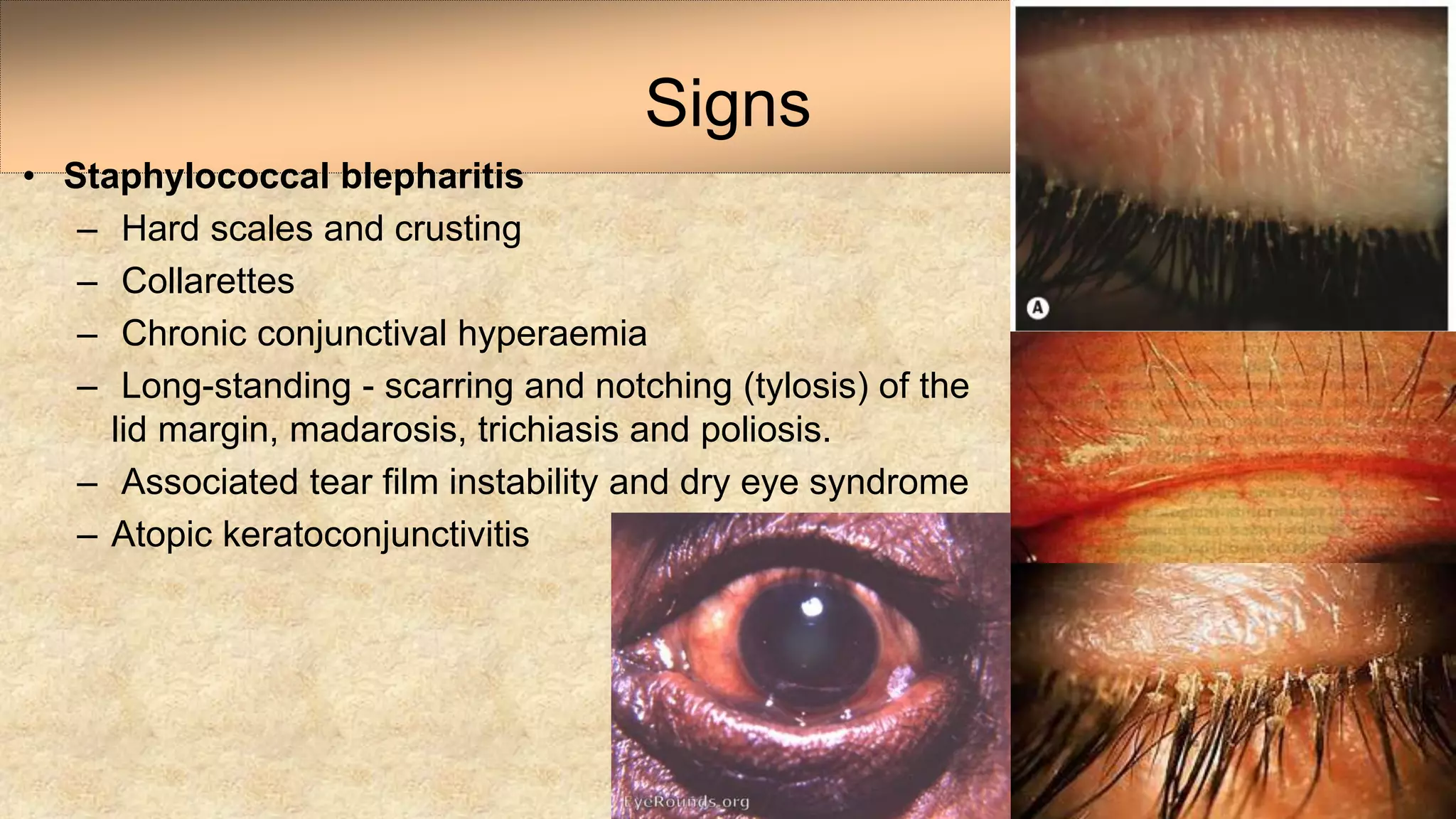
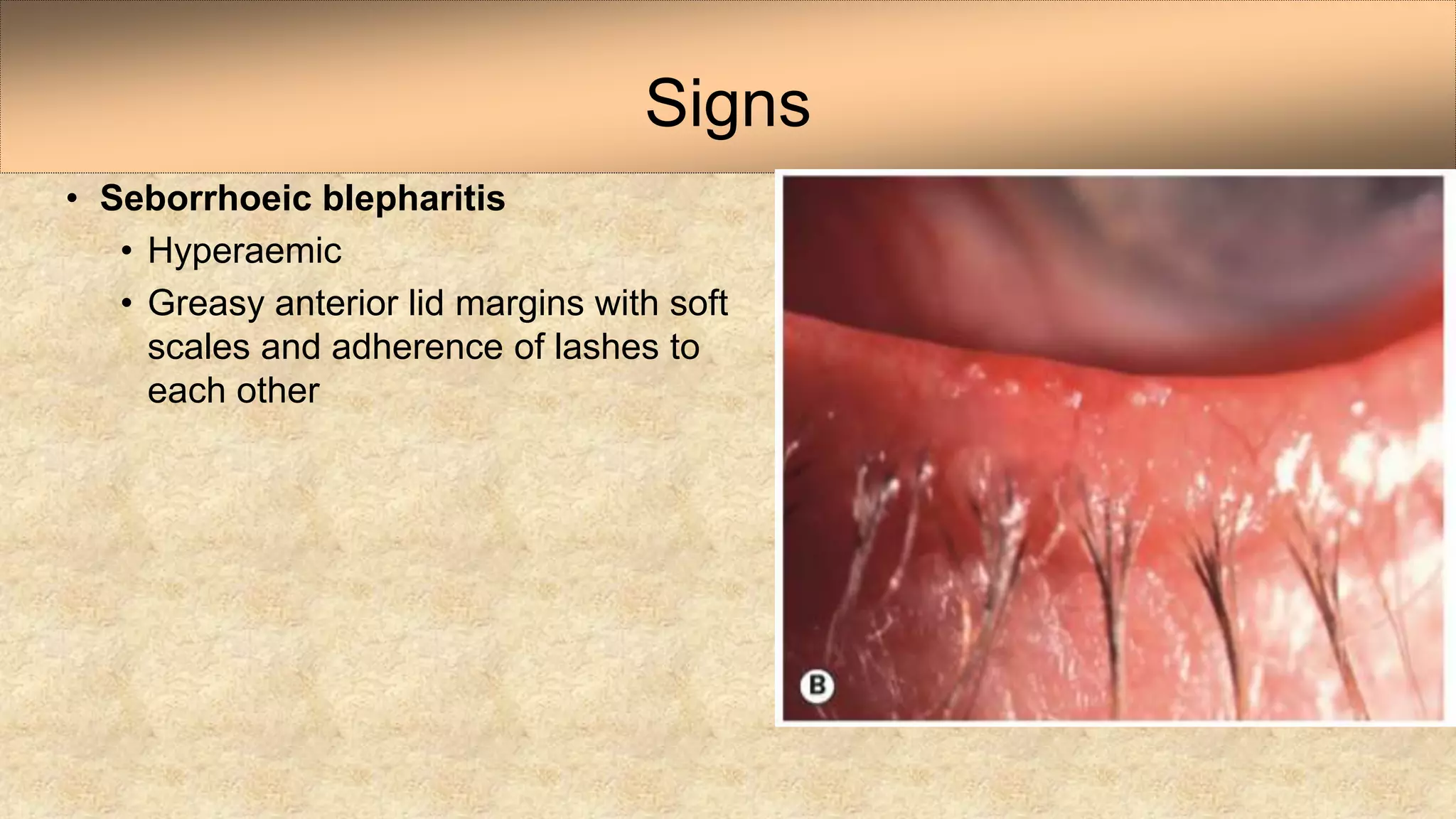
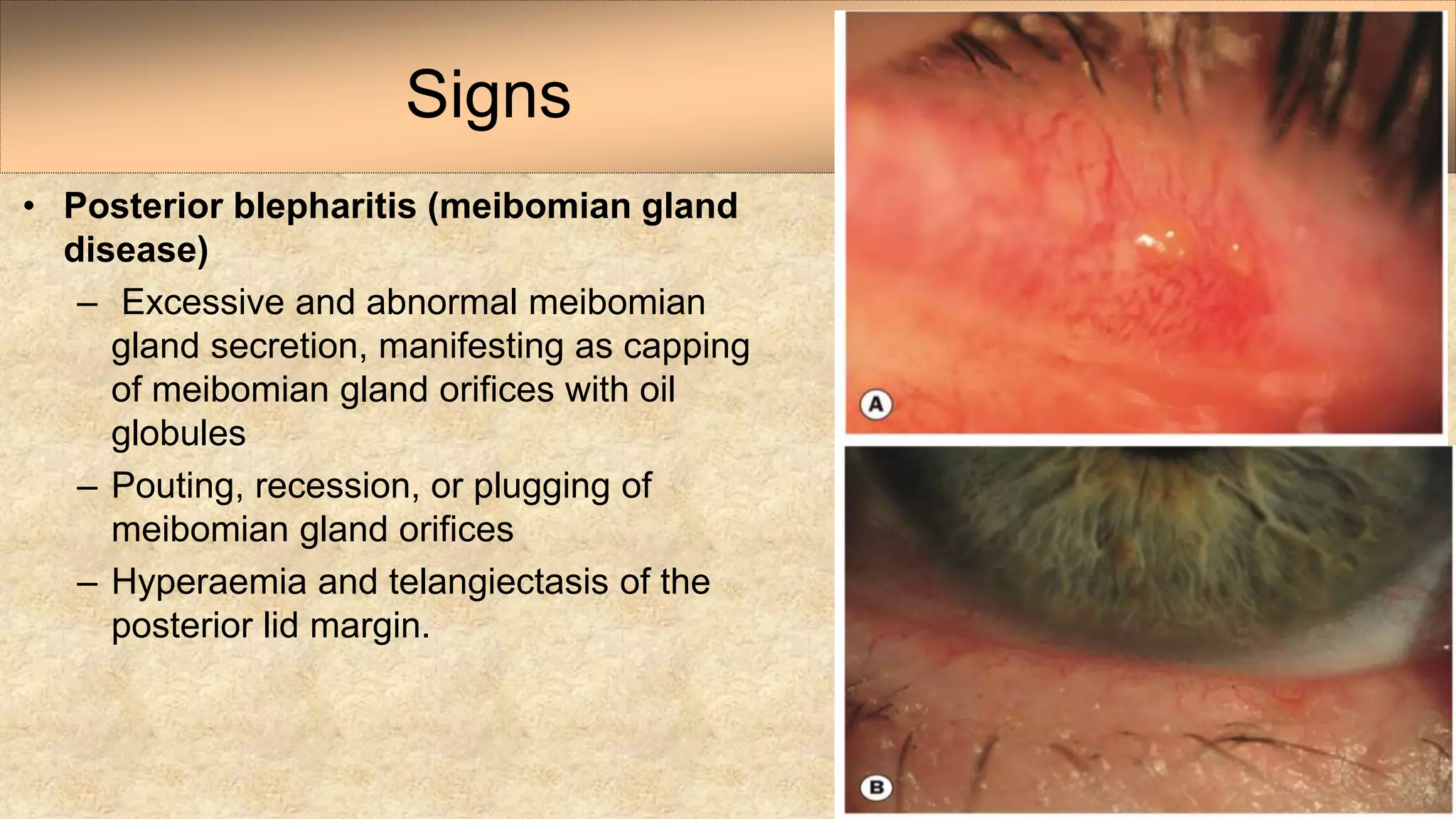
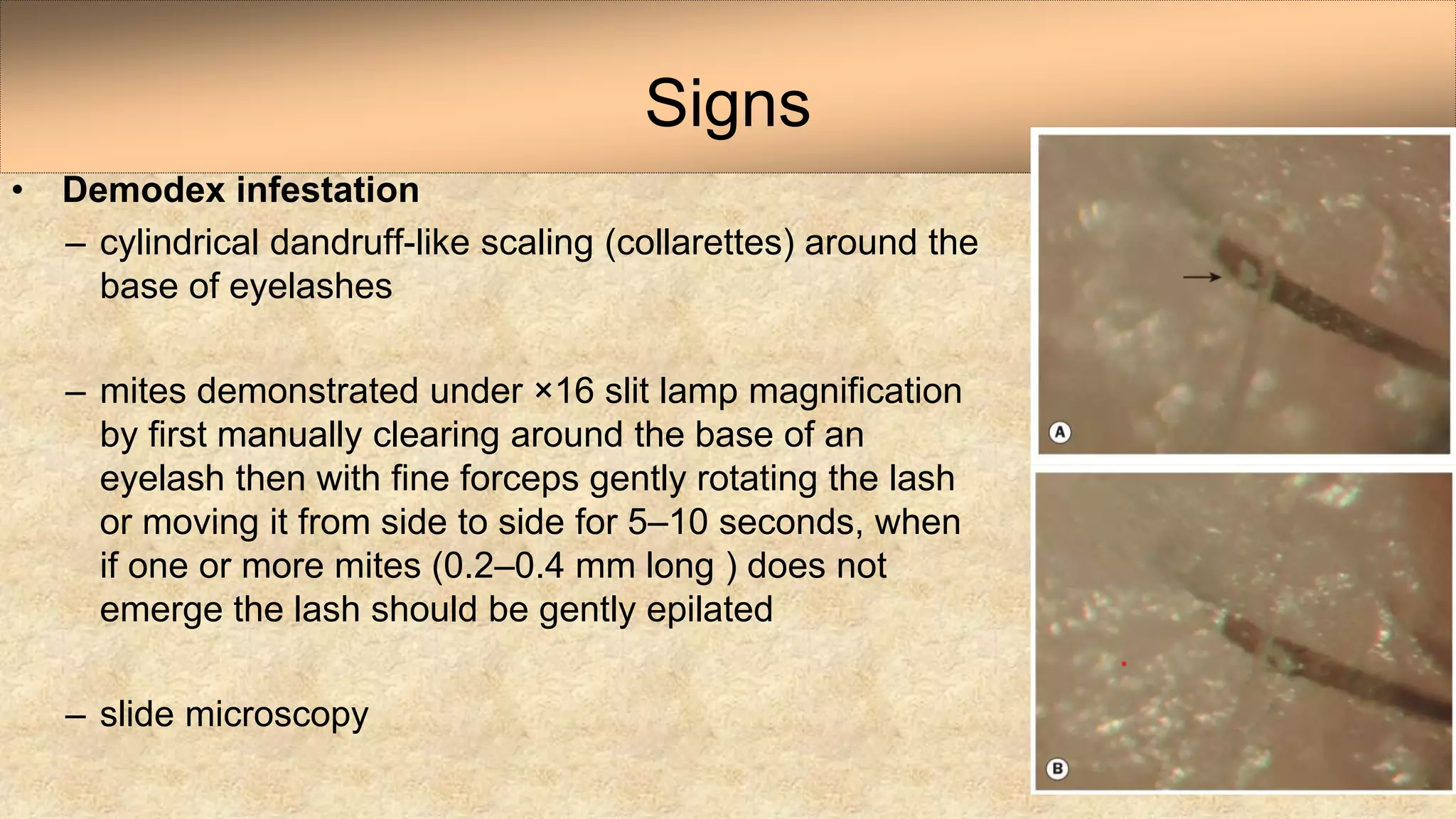
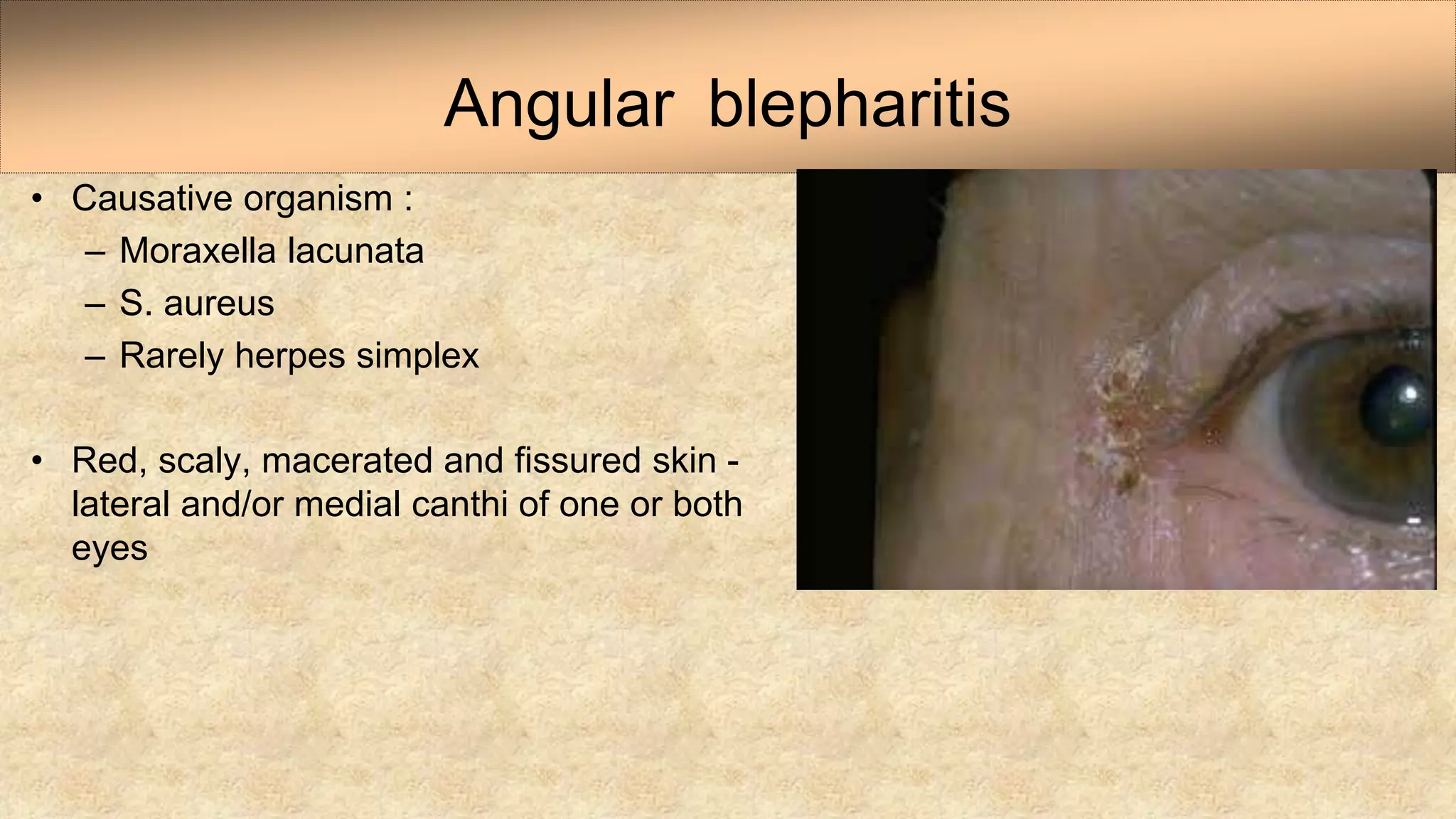
This document discusses bacterial infections and blepharitis that can affect the eyelids. It begins by covering the anatomy of the eyelid and then describes several specific bacterial infections including external hordeolum, impetigo, erysipelas, necrotizing fasciitis, anthrax, and syphilis. It then discusses blepharitis in detail, describing the different types (staphylococcal, seborrheic, posterior), associated conditions like meibomian gland dysfunction, symptoms, signs, treatment, and complications.