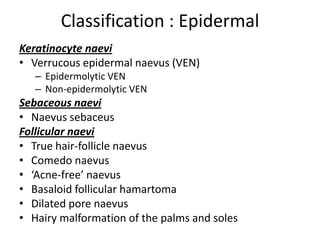
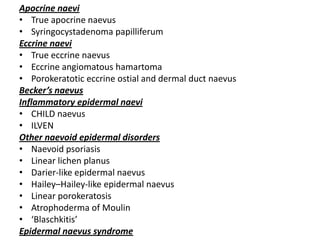
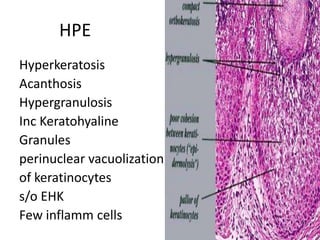
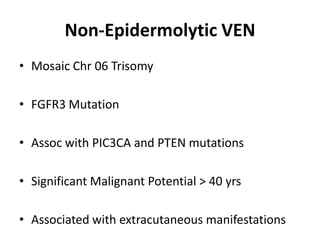
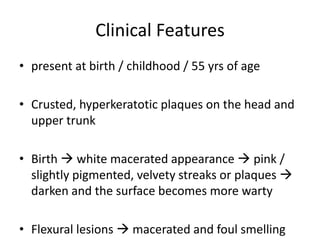
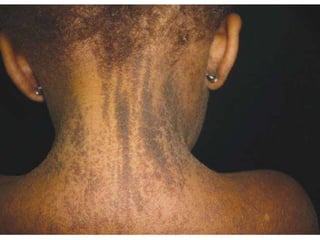
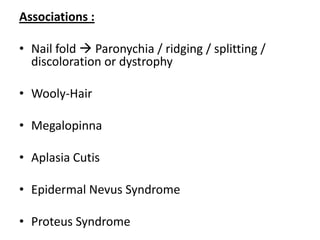
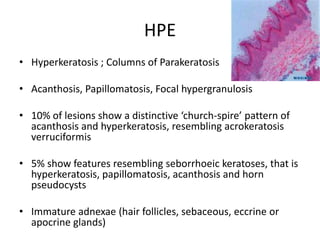
This document discusses epidermal naevi, which are congenital developmental defects or birthmarks of the skin and mucosa. It describes different types of epidermal naevi classified based on the level of defect (epidermal, dermal, subcutaneous) and component cell (vascular, connective tissue, melanocytic). Verrucous epidermal naevi, also known as verrucous nevus or nevus verrucosus, are discussed in detail. They are keratinocyte hamartomas that can be either epidermolytic or non-epidermolytic types, with the latter having greater malignant potential and possible associations with extracutaneous abnormalities. Clinical features