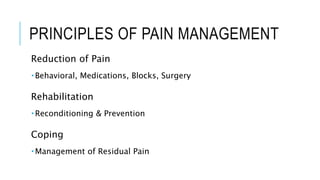
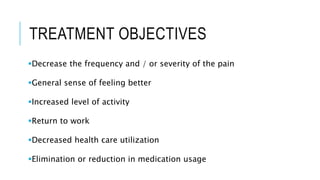
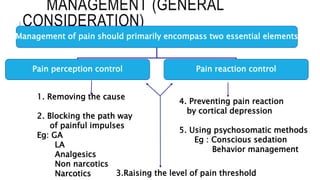
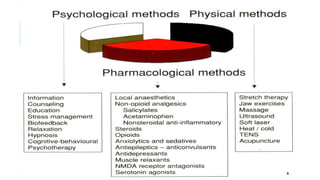
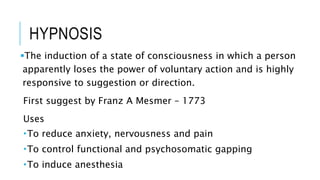
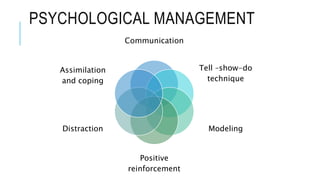
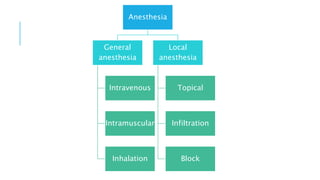
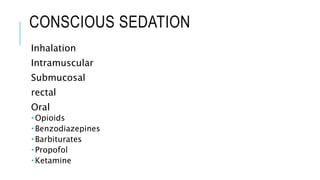
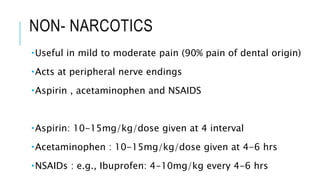
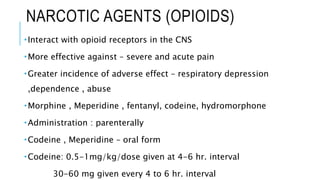
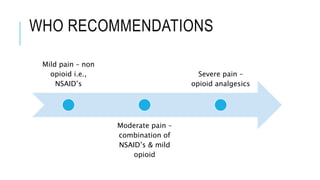
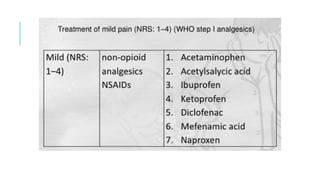
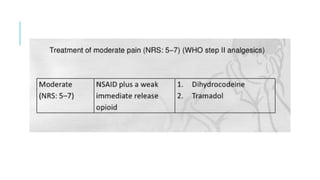
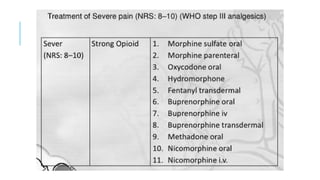
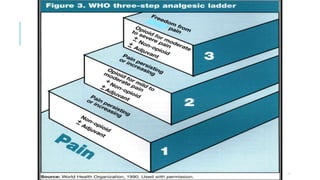
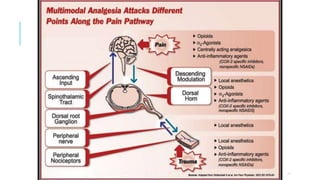
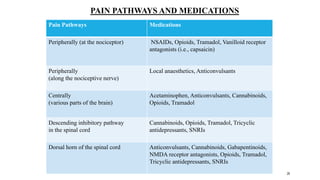
Dr. Dharati outlines principles and methods for effective pain management, emphasizing the importance of understanding pain perception and reaction to control pain effectively. The document details various treatments, including behavioral strategies, medications, physical therapy, and surgical options to alleviate pain and improve patient quality of life. It concludes that proper diagnosis and understanding of pain sources are essential for developing a successful treatment plan.