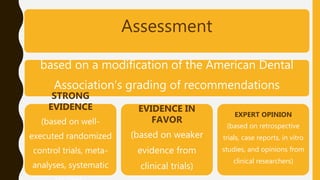
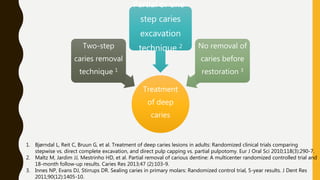
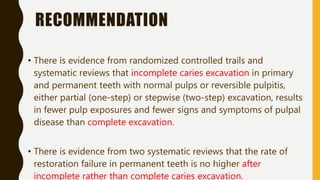
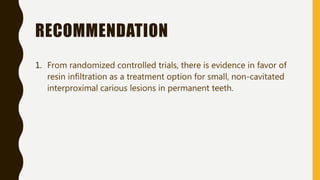
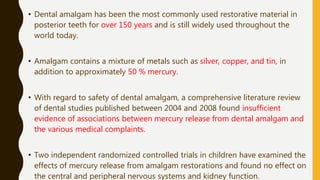
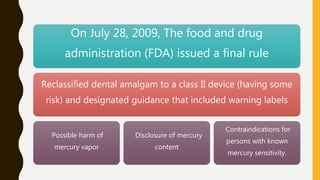
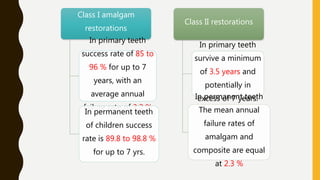
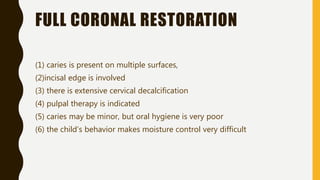
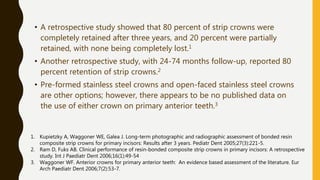
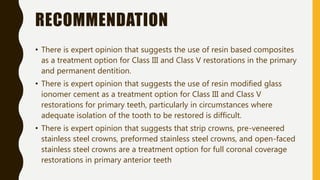
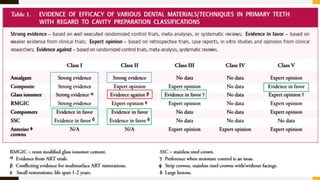
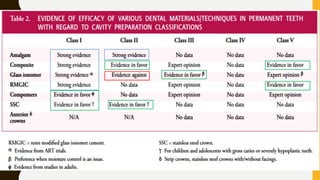
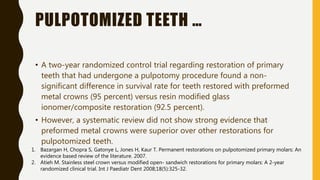
The AAPD guidelines for restorative dentistry provide recommendations on the necessary treatments, materials, and techniques for managing dental caries, focusing on evidence from research studies. Key recommendations include the management of carious lesions based on an individual's risk, appropriate use of dental sealants for prevention, and the effectiveness of incomplete caries excavation techniques. The document emphasizes the importance of maintaining pulpal vitality in treatment, the need for careful assessment of restoration methods, and ongoing monitoring for the success of dental interventions.