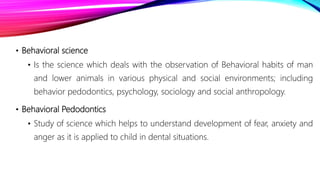
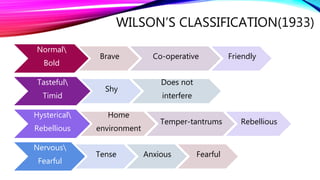
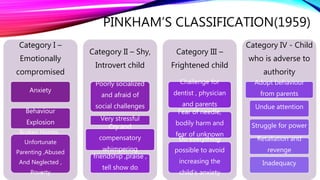
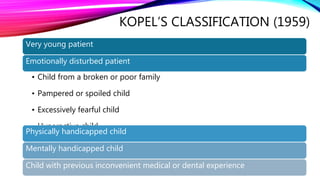
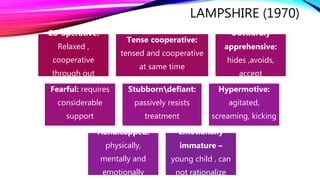
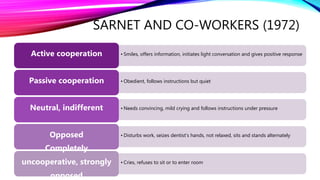
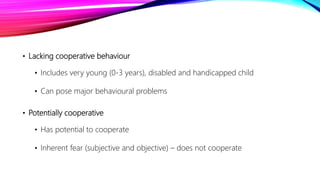
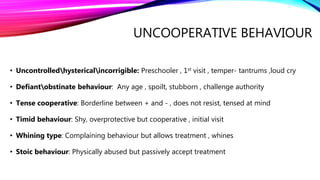
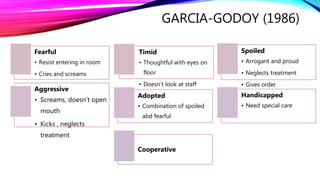
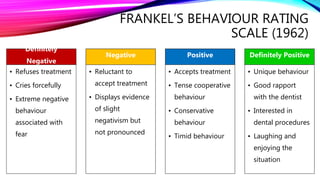
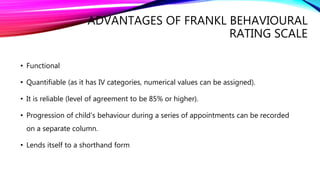
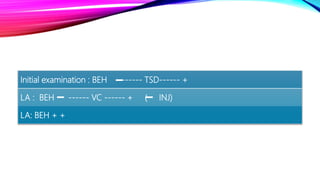
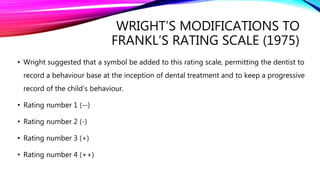
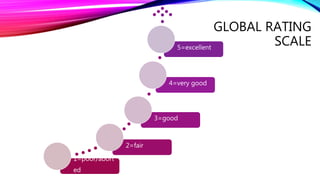
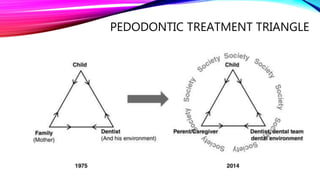
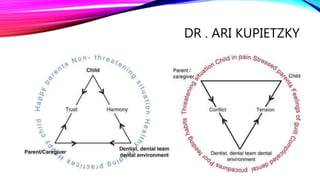
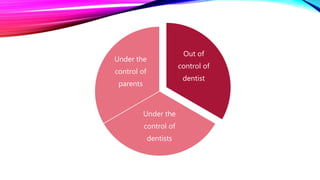
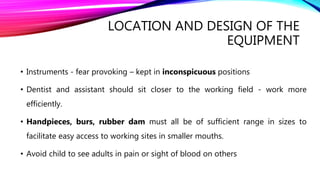
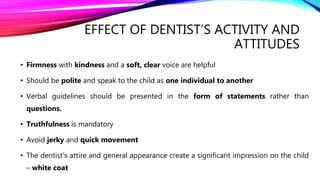
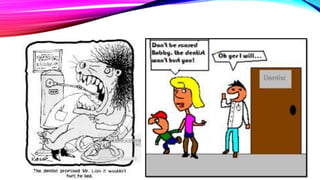
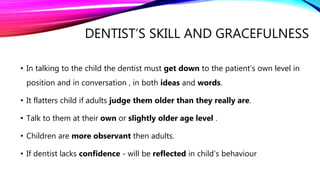
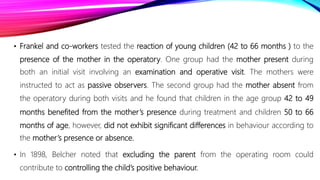
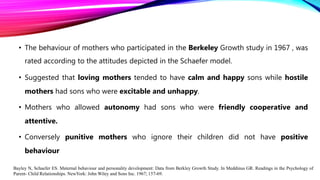
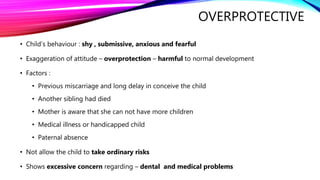
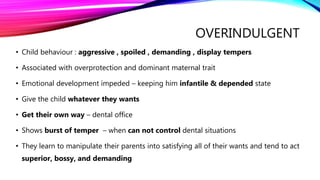
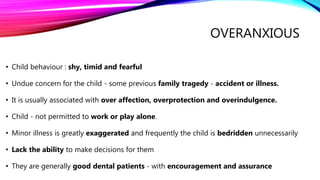
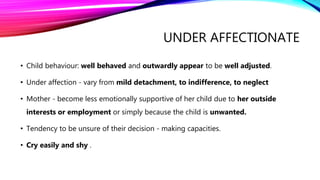
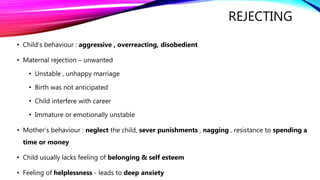
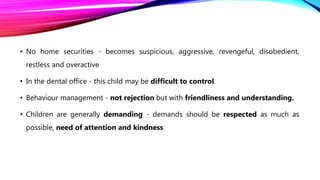
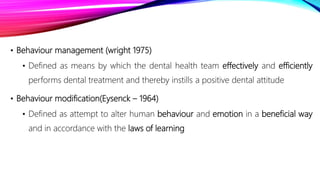
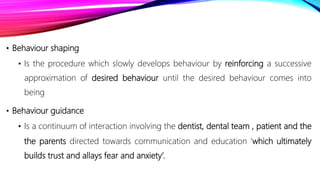
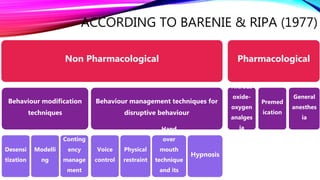
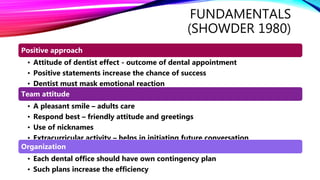
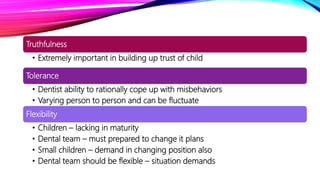
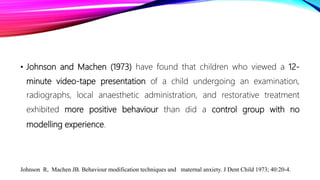
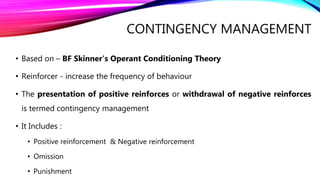
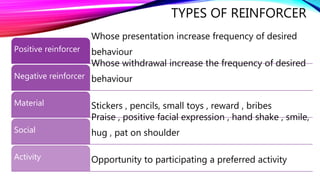
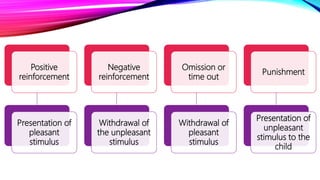
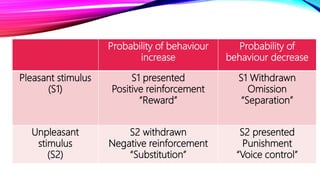
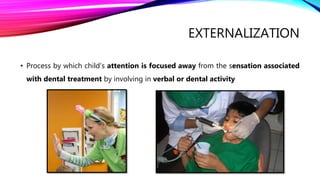
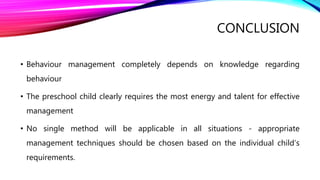
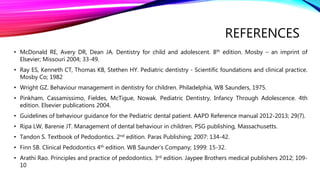
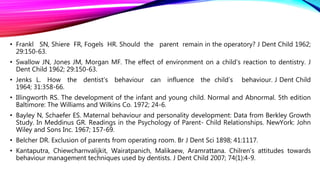
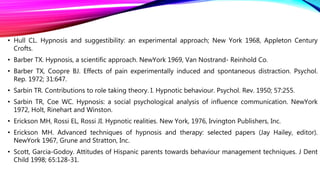
The document focuses on the application of behavioral sciences in pediatric dentistry, discussing definitions and classifications of child behavior in dental clinics. It outlines various factors affecting children's behavior such as parental influence, the dental environment, and previous experiences, along with behavioral rating scales for managing these behaviors. The text emphasizes the importance of understanding child behavior to enhance effective communication and treatment strategies in pediatric dentistry.
![DEFINITIONS
• Behaviour
• Any activity that can be observed, recorded and measured.
• Any change observed in functioning of an organism.
• Behaviour is the sum total of response to stimuli, internal and external
[Healy, Bronner and Bowers, 1965]
• Behaviour is defined as the response by the child and the reaction of the
dentist as the consequence. The consequence can be answered with a
reinforcer, which strengthens behaviour in a patient, or with a punisher, which
weakens behaviour [Rosenberg, 1974]](https://image.slidesharecdn.com/behaviouralsciencesanditsapplicationtopedodontics-210418163619/85/Behavioural-sciences-and-its-application-to-pedodontics-4-320.jpg)