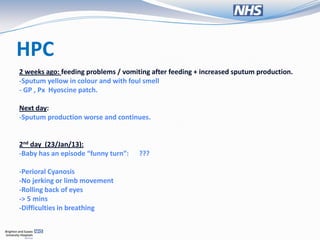
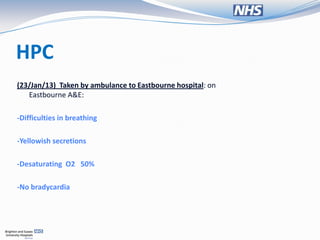
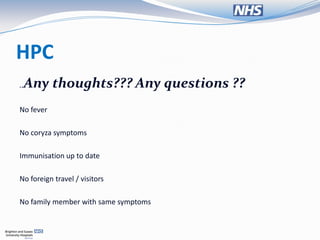
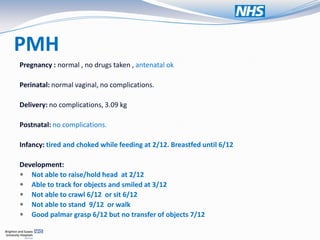
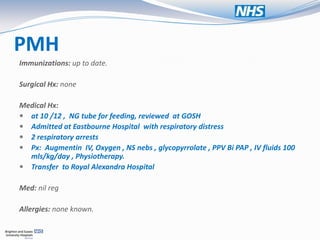
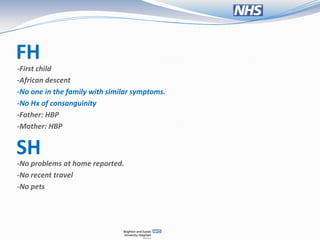
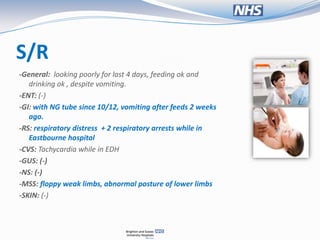
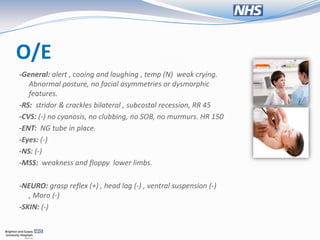
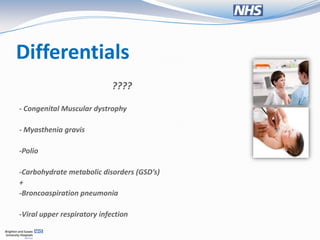
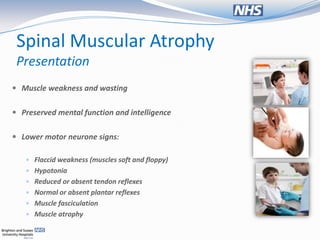
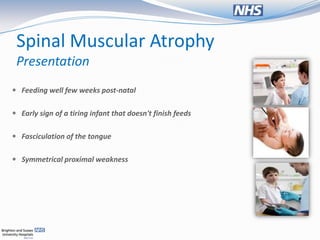
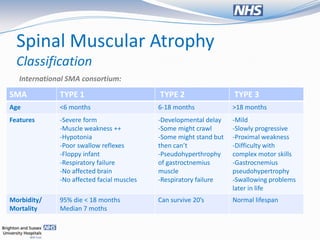
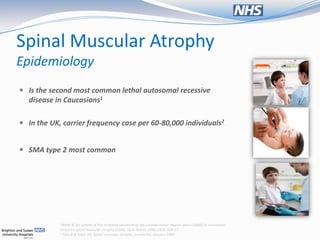
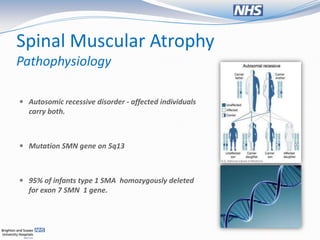
The document presents a case study of a 13-month-old female with respiratory distress and symptoms suggestive of spinal muscular atrophy (SMA), detailing her medical history, physical examination, and diagnostic challenges. It discusses the pathophysiology, classification, and management of SMA, as well as ethical considerations regarding ventilatory support for affected patients. The document emphasizes the importance of a multidisciplinary approach in providing care and the varied perspectives among clinicians about the quality of life for children with SMA.