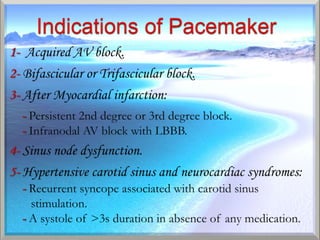
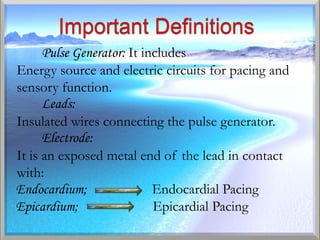
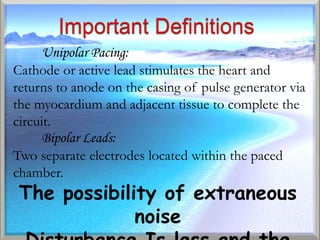
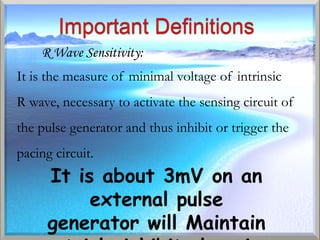
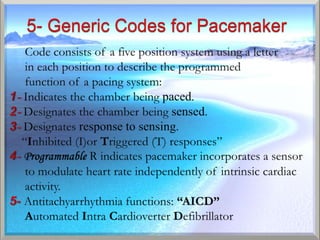
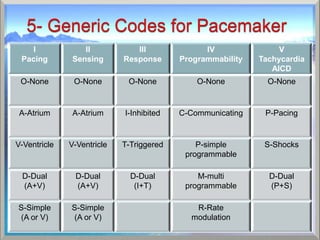
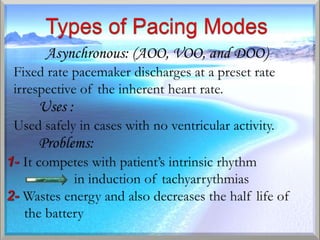
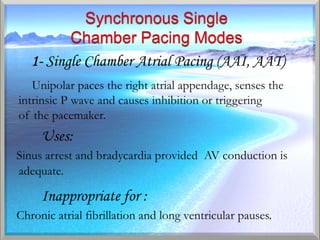
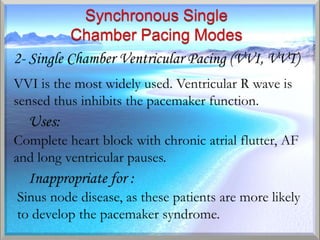
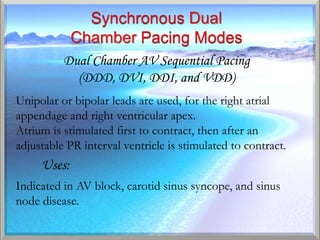
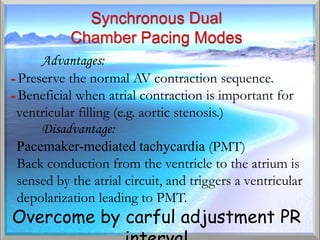
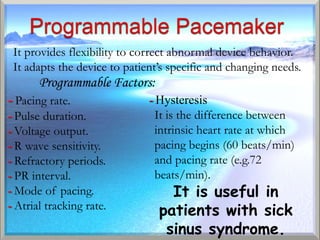
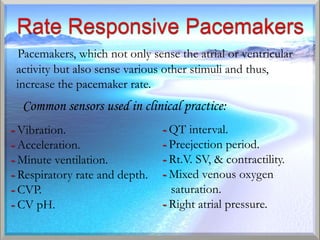
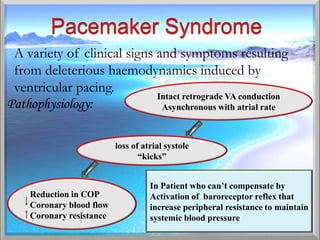
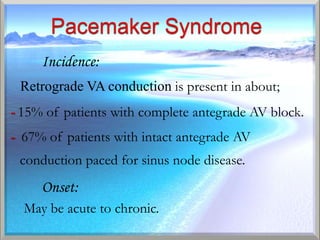
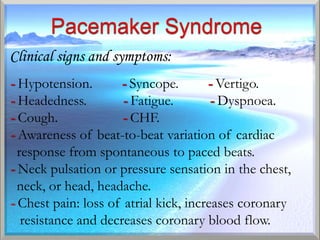
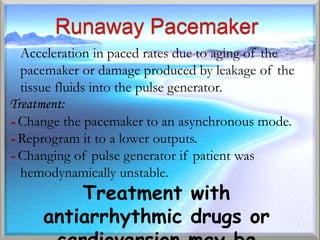
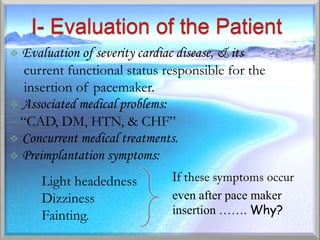
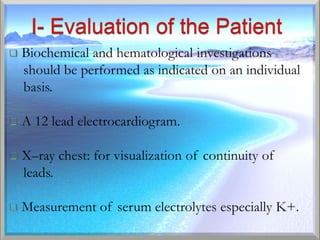
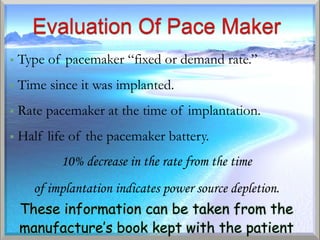
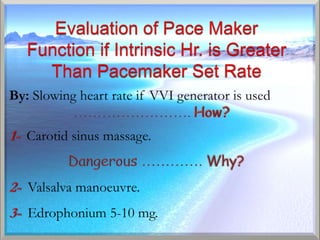
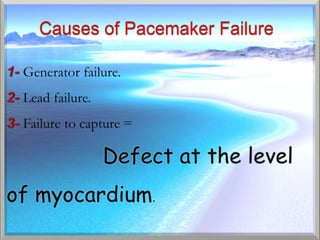
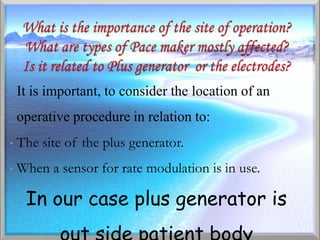
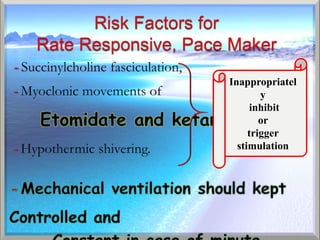
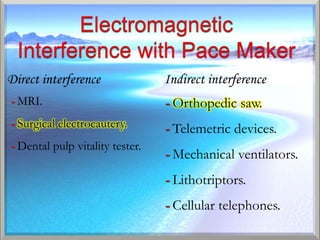
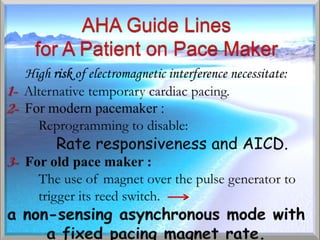
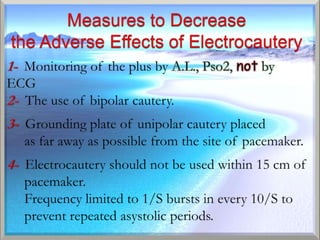
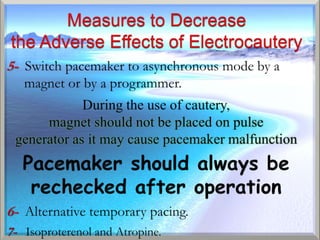
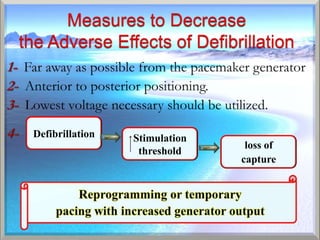
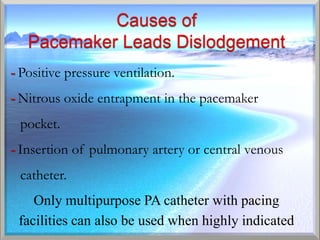
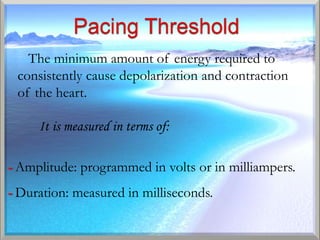
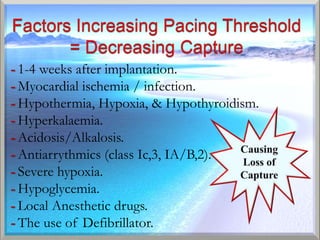
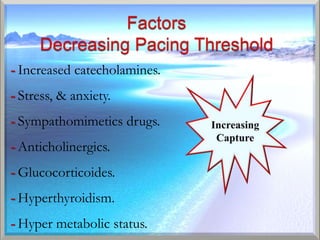
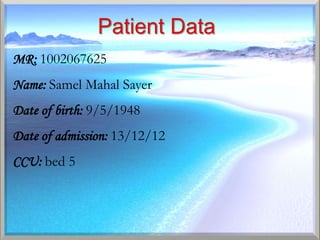
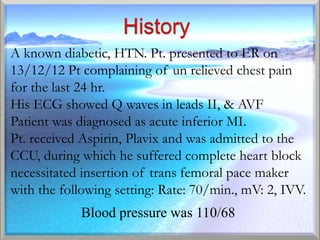
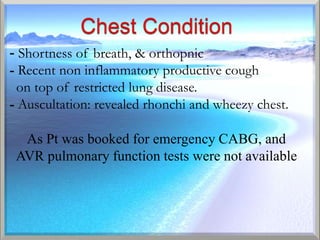
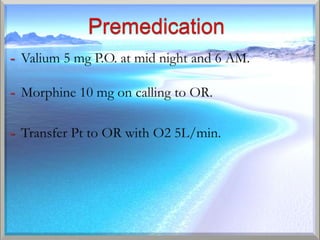
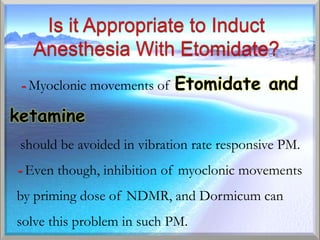
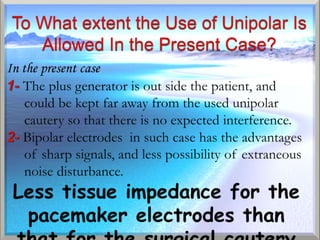
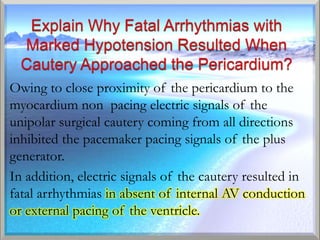
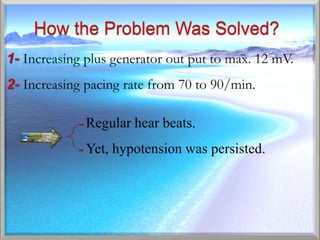
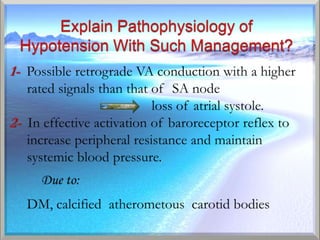
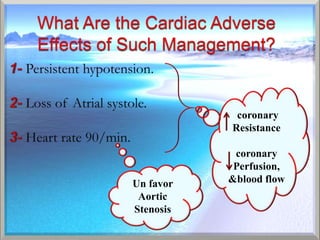
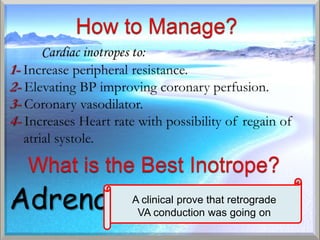
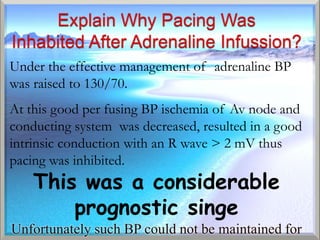
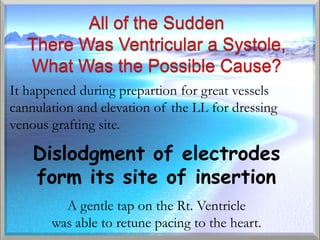
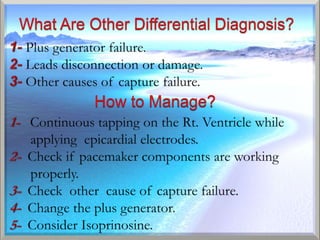
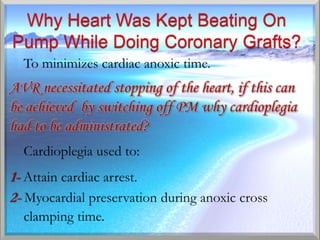
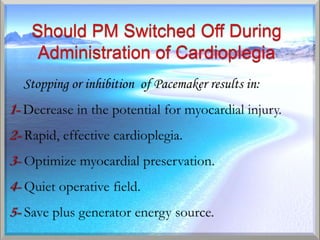
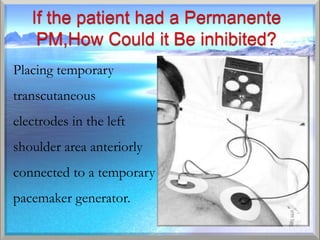
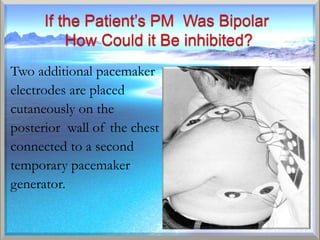
This document discusses pacemakers, including their history, components, types, functions, programming, complications, and clinical management. It provides details on pacemaker technology, how they treat arrhythmias, and considerations for patients with pacemakers during medical procedures or surgery.