A cardiac pacemaker is a small device implanted in a person’s chest that provides an electrical pulse to the heart, as needed, to regulate a slow heart rate.
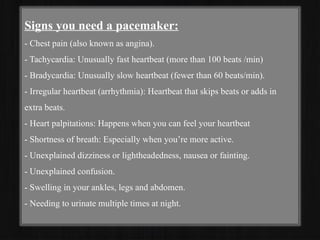
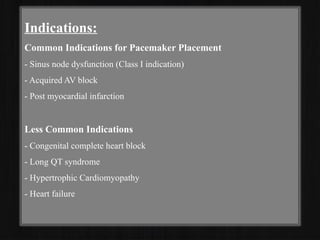
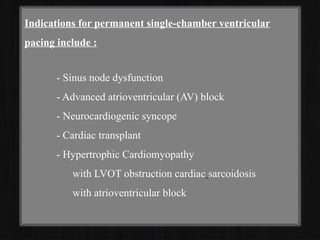
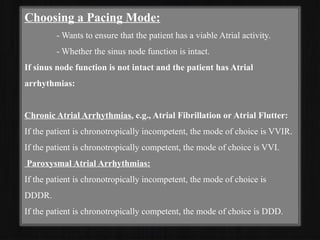
As people age, some may experience a slower-than-normal heart rate caused by electrical problems or blockages within the heart. When the heart rate slows considerably, it can cause worrisome symptoms, such as dizziness and shortness of breath. A pacemaker can help to restore a person’s slow heart rate to a normal one, reducing or eliminating these symptoms.The heart runs on electrical activity. In a healthy person, the part of the heart that naturally maintains rhythm is called either the sinus node or sinoatrial node. This “natural pacemaker” sends electrical signals through the heart that make its upper chambers contract, pushing blood through to its lower chambers and keeping the heart beating at a normal rhythm.
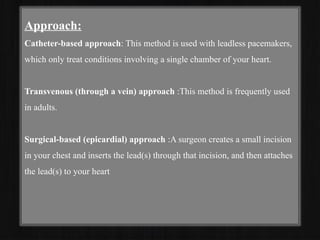
Sometimes, however, the sinus node stops working efficiently. It may lose momentum, which slows down a person’s heart rate, or a blockage may develop in the heart, which slows down or disrupts the electrical pulses traveling through the heart. In both instances, a pacemaker may be needed to help a person’s slow heart rate resume to a normal, steady speed. Once implanted, the device may last up to 15 years before it needs to be replaced.
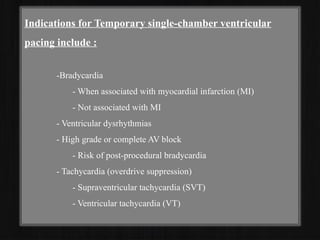
Although pacemakers may sometimes be used as a temporary measure, such as during a medical emergency, they typically remain permanently in place.
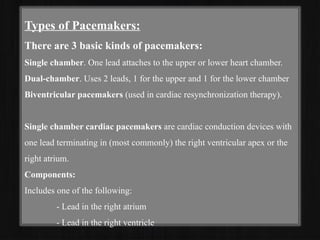
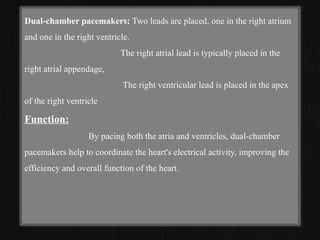
Some pacemakers, called biventricular pacemakers, can treat heart failure. They may also operate as implantable cardioverter defibrillators, designed to shock the heart and return it to a normal rhythm when it beats too quickly or