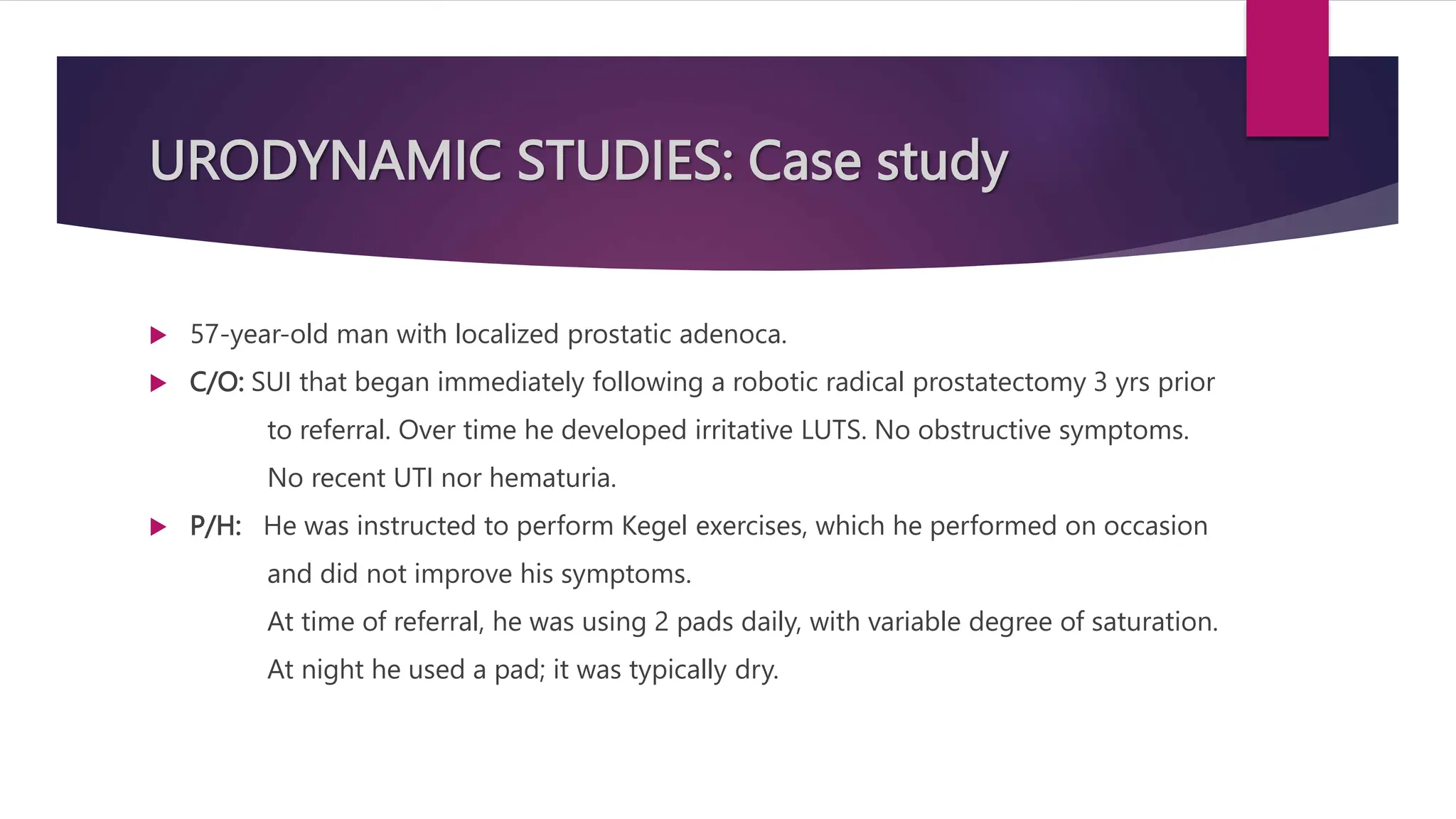
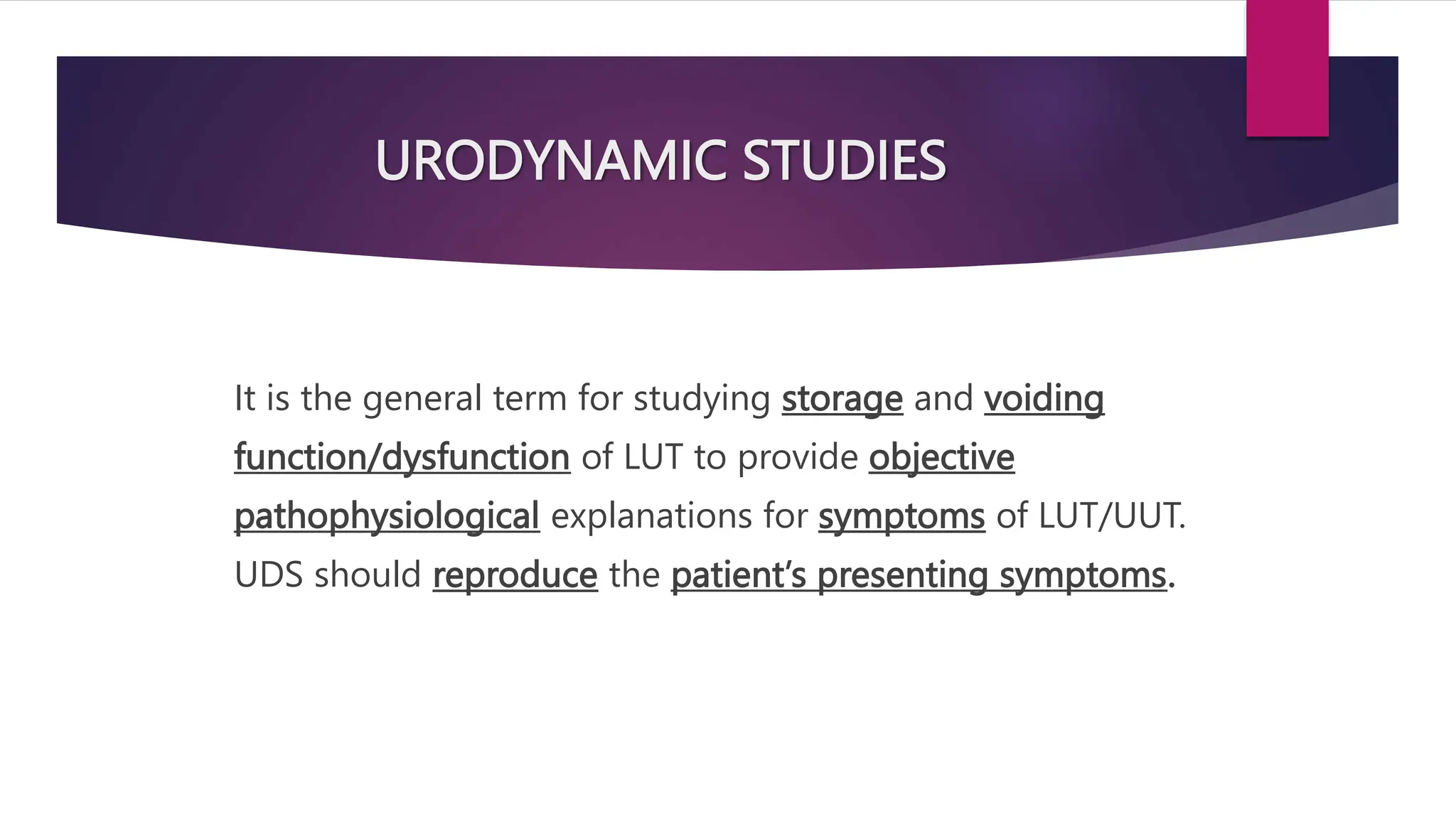
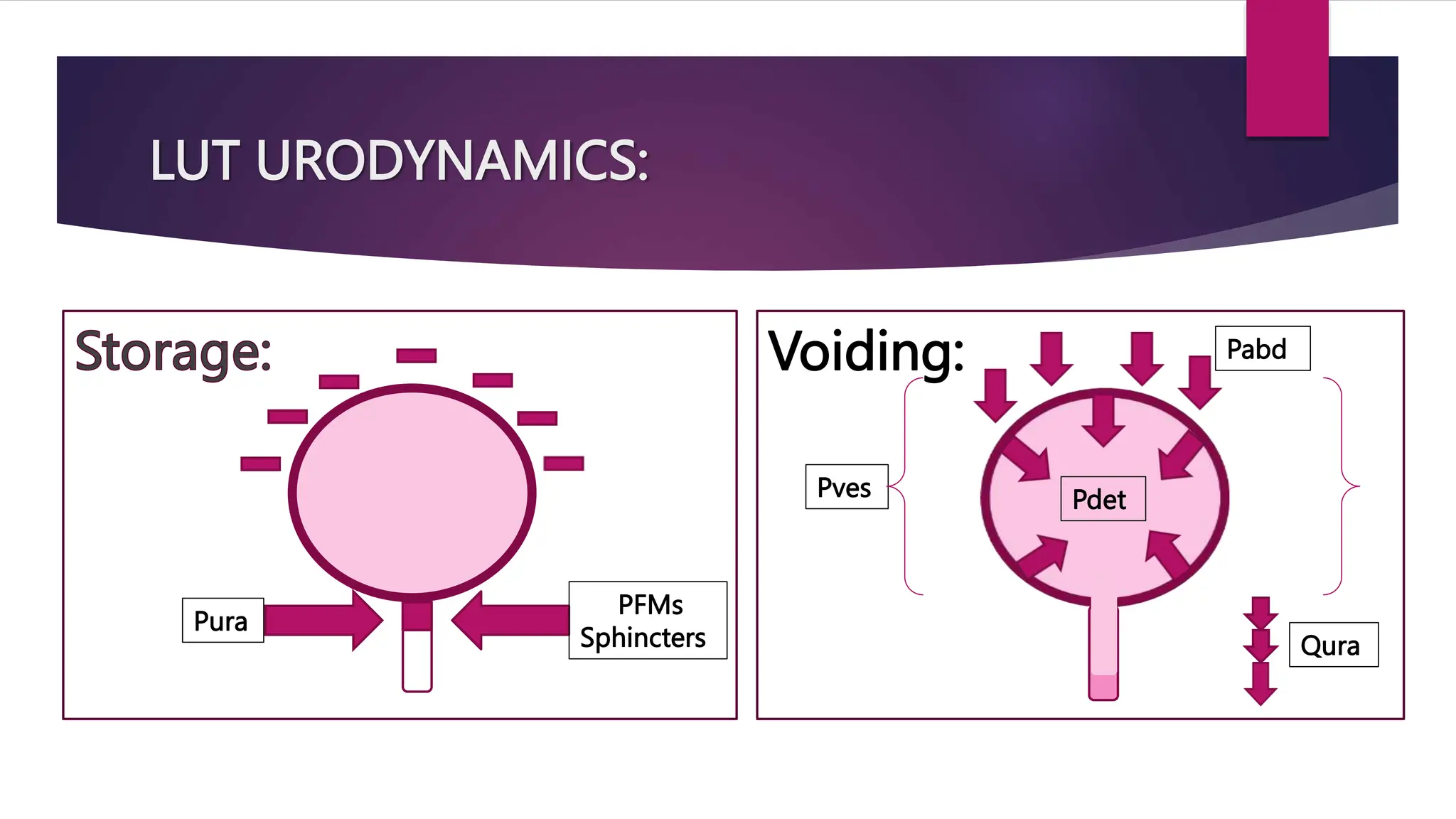
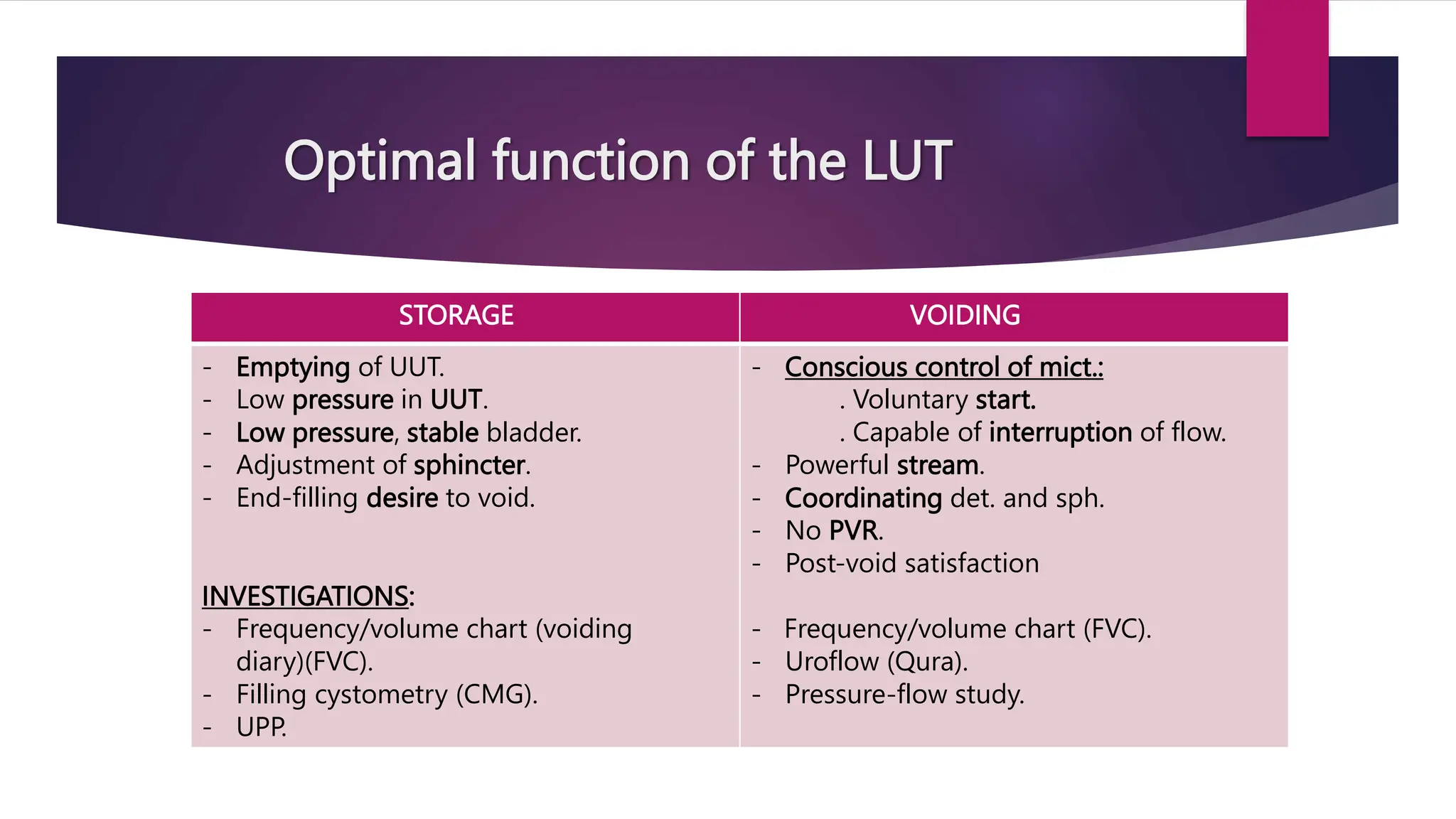
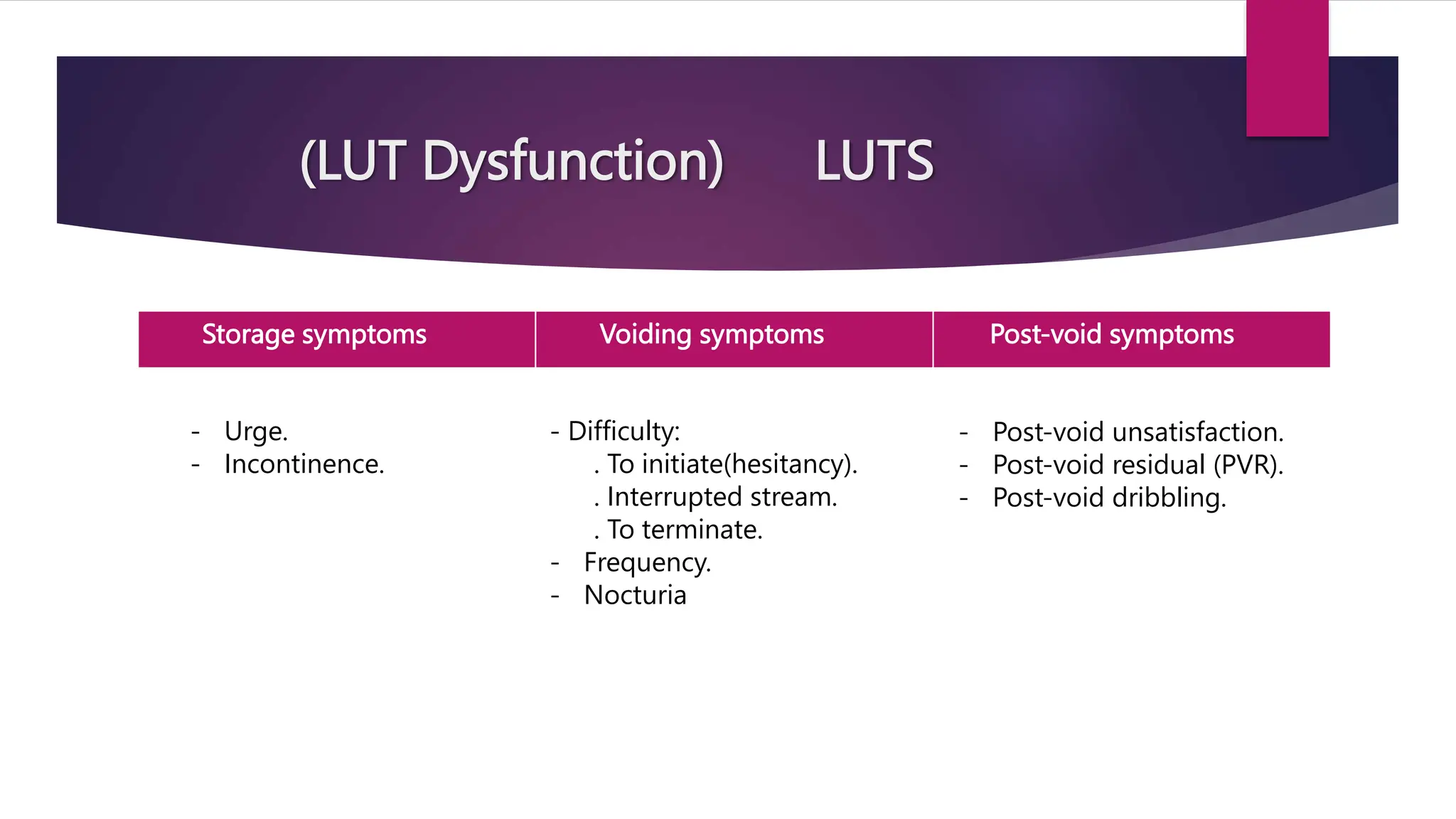
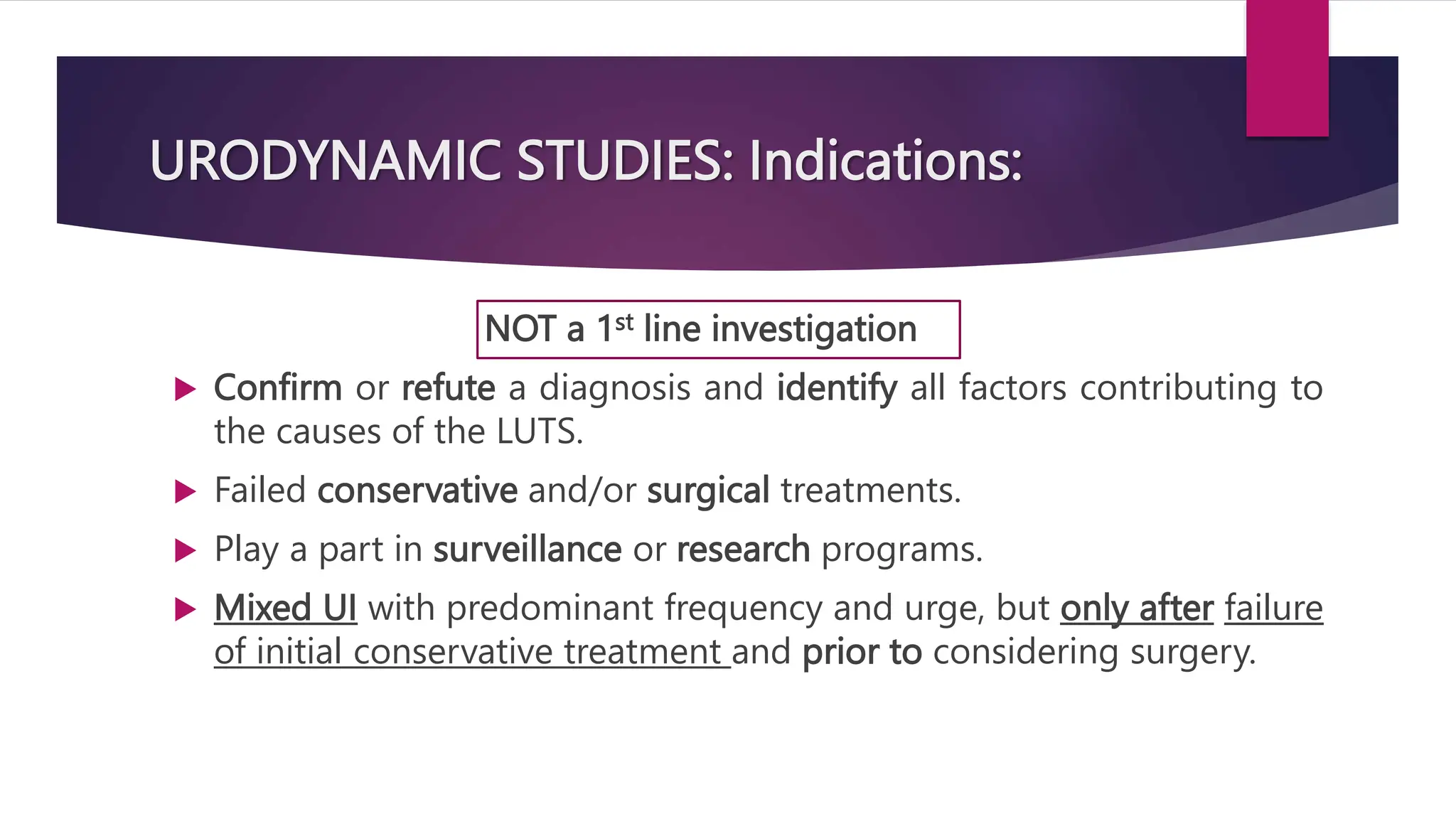
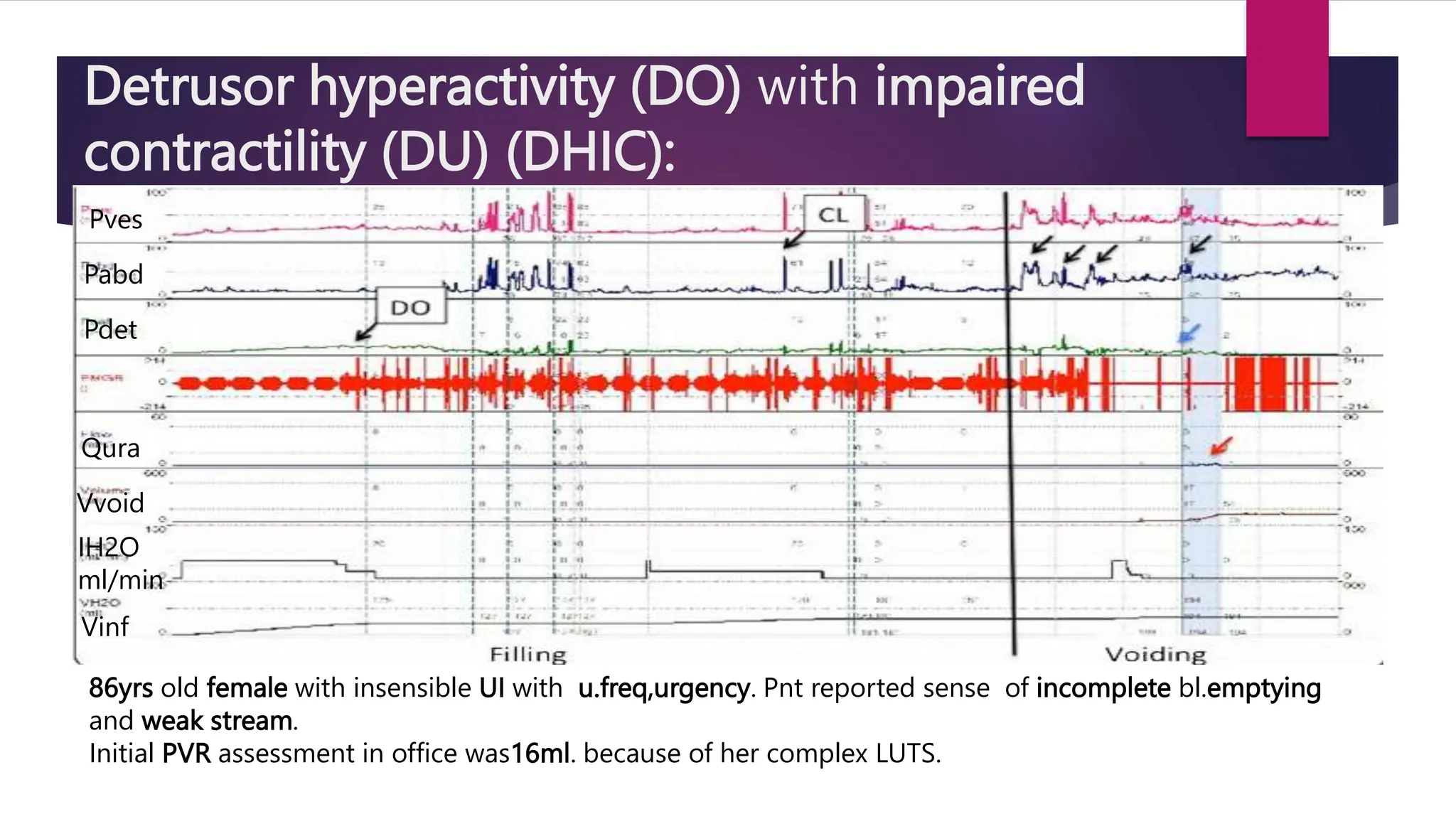
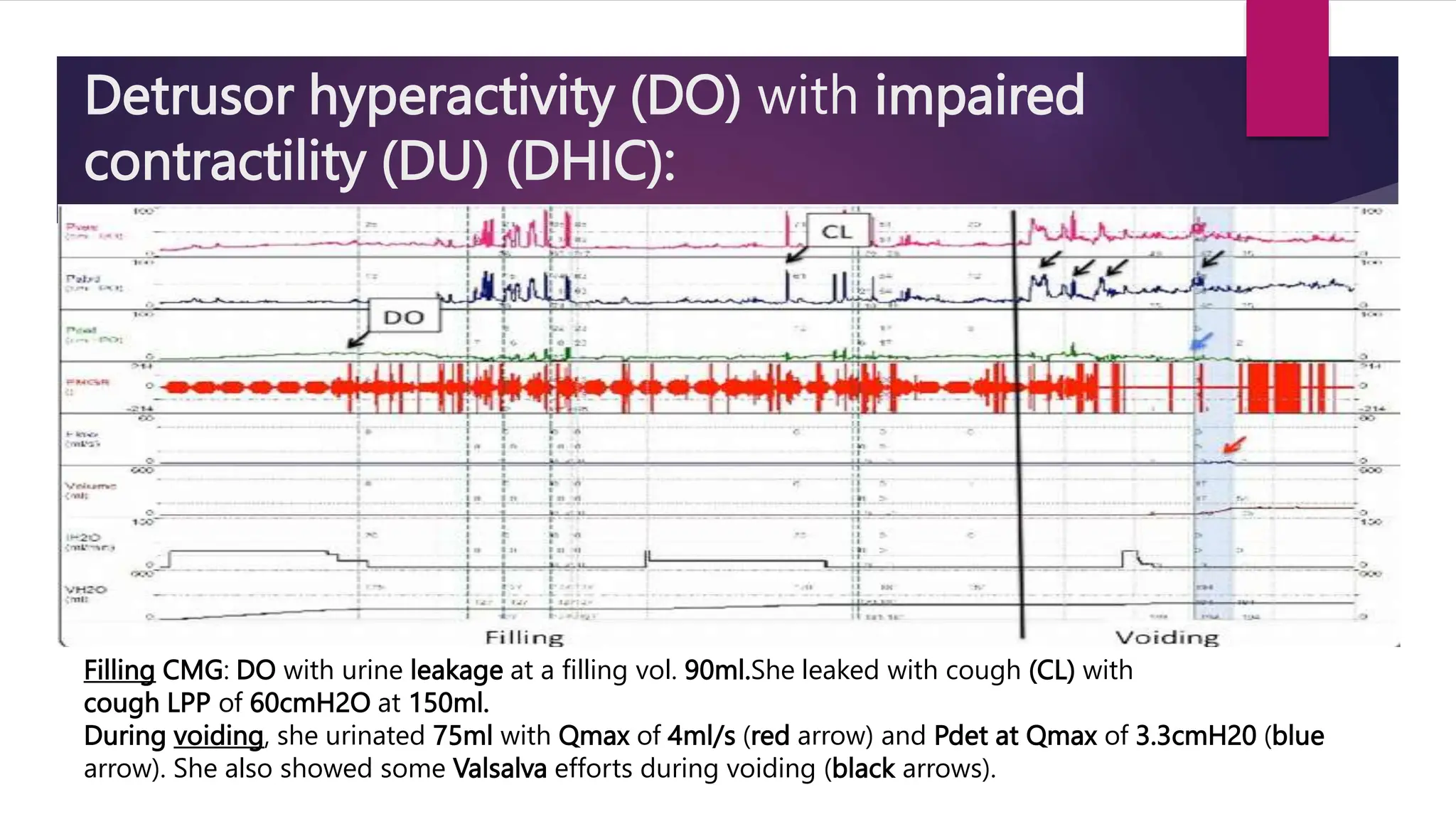
Urodynamic studies assess the storage and voiding functions of the lower urinary tract to provide objective explanations for related symptoms. The studies include various tests, such as filling cystometry and pressure-flow studies, and utilize patient diaries to track urinary habits. Indications for these studies include failure of conservative treatments and to confirm diagnoses of lower urinary tract symptoms.

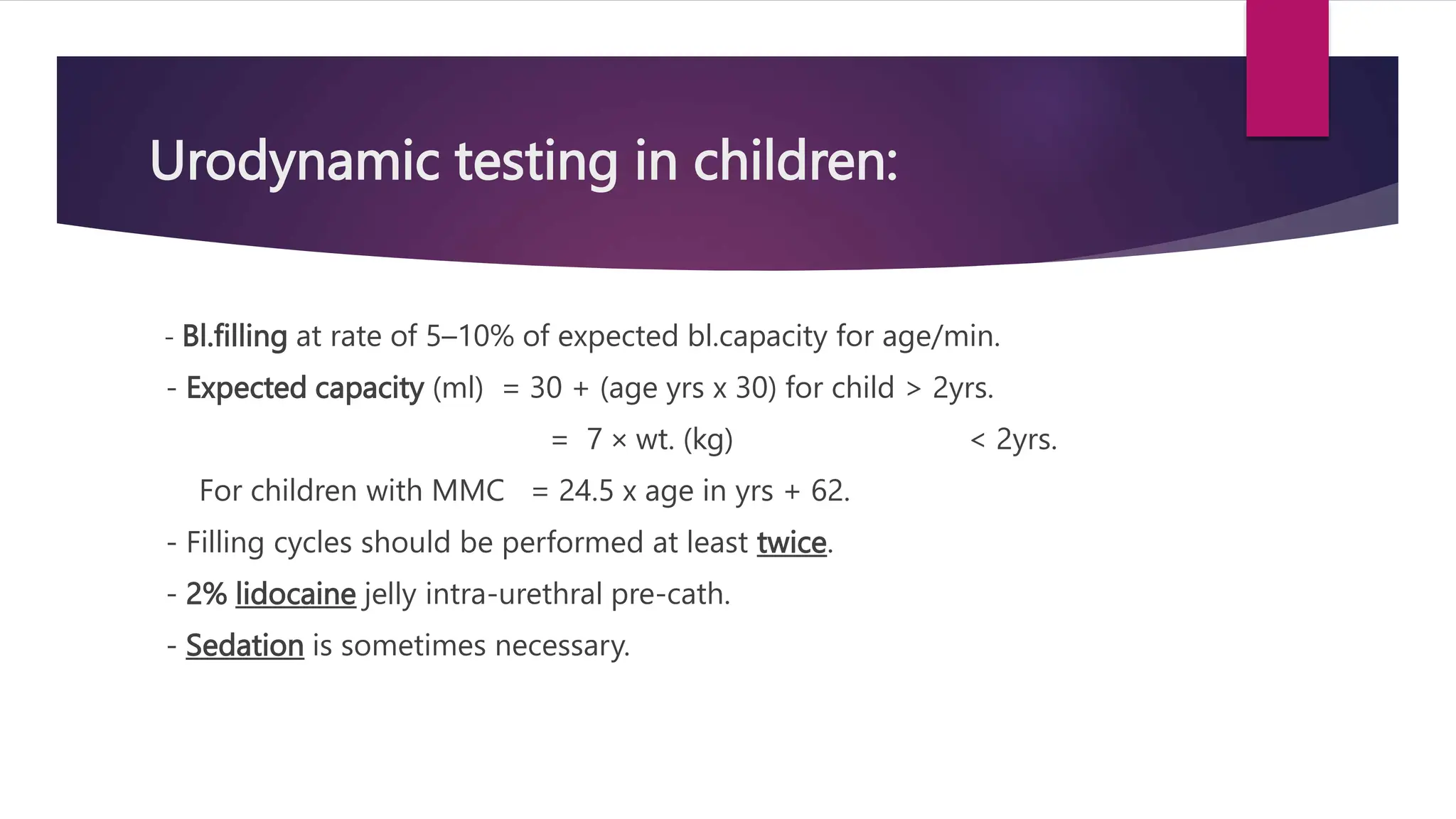
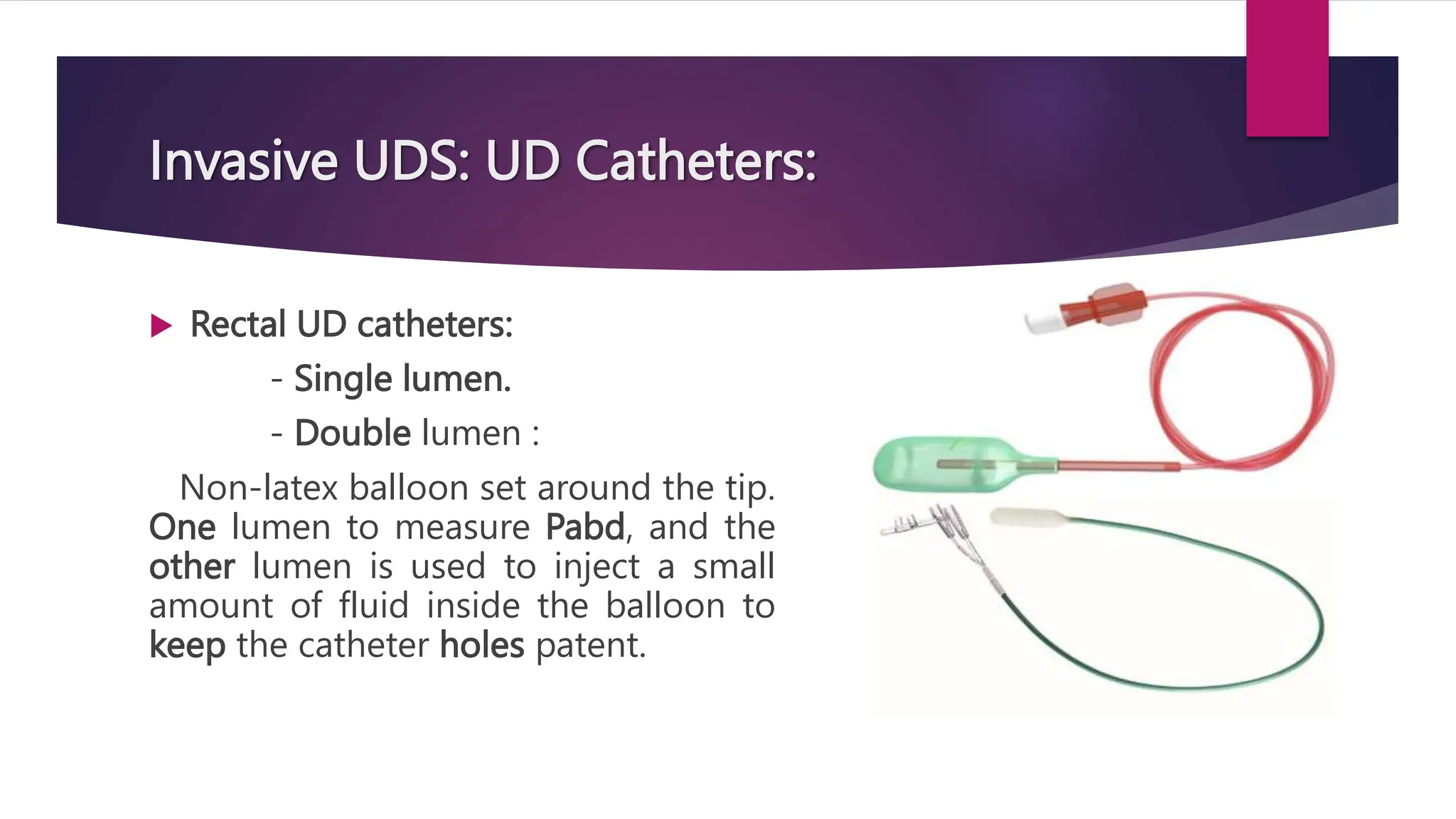
![Residual urine volume ( PVR ):
- In infants: PVR volume < 10% of the max. bl. vol. is
considered normal.
Voided percentage (Void%):
The numerical description of the voiding efficacy (VE)
which is the proportion of bladder content emptied.
Calculation: [vol. voided / vol. voided + PVR] x 100.](https://image.slidesharecdn.com/urodynamicstudies-231212121037-ac38053d/75/Urodynamic-studies-overview-and-examples-pptx-53-2048.jpg)
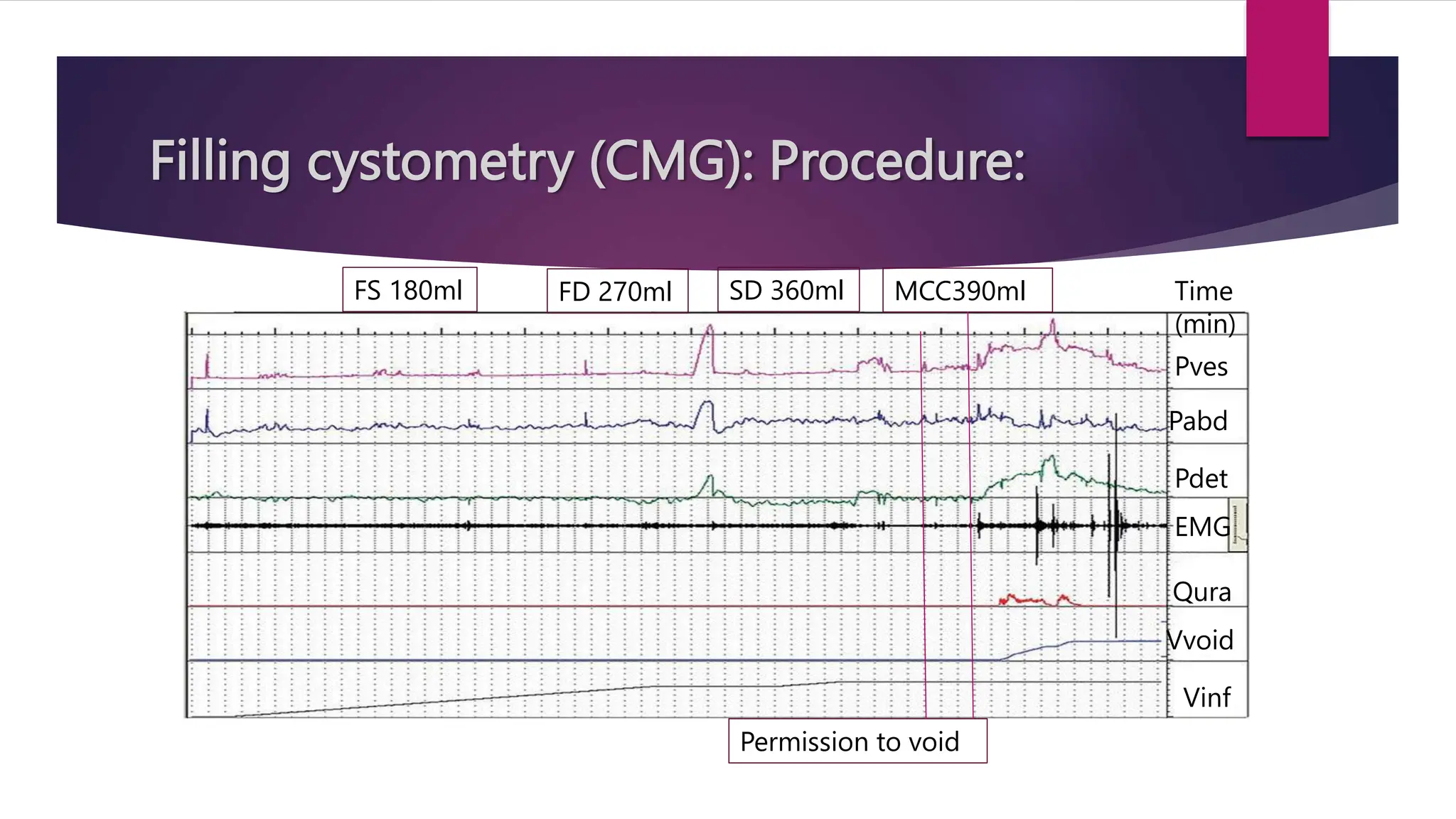


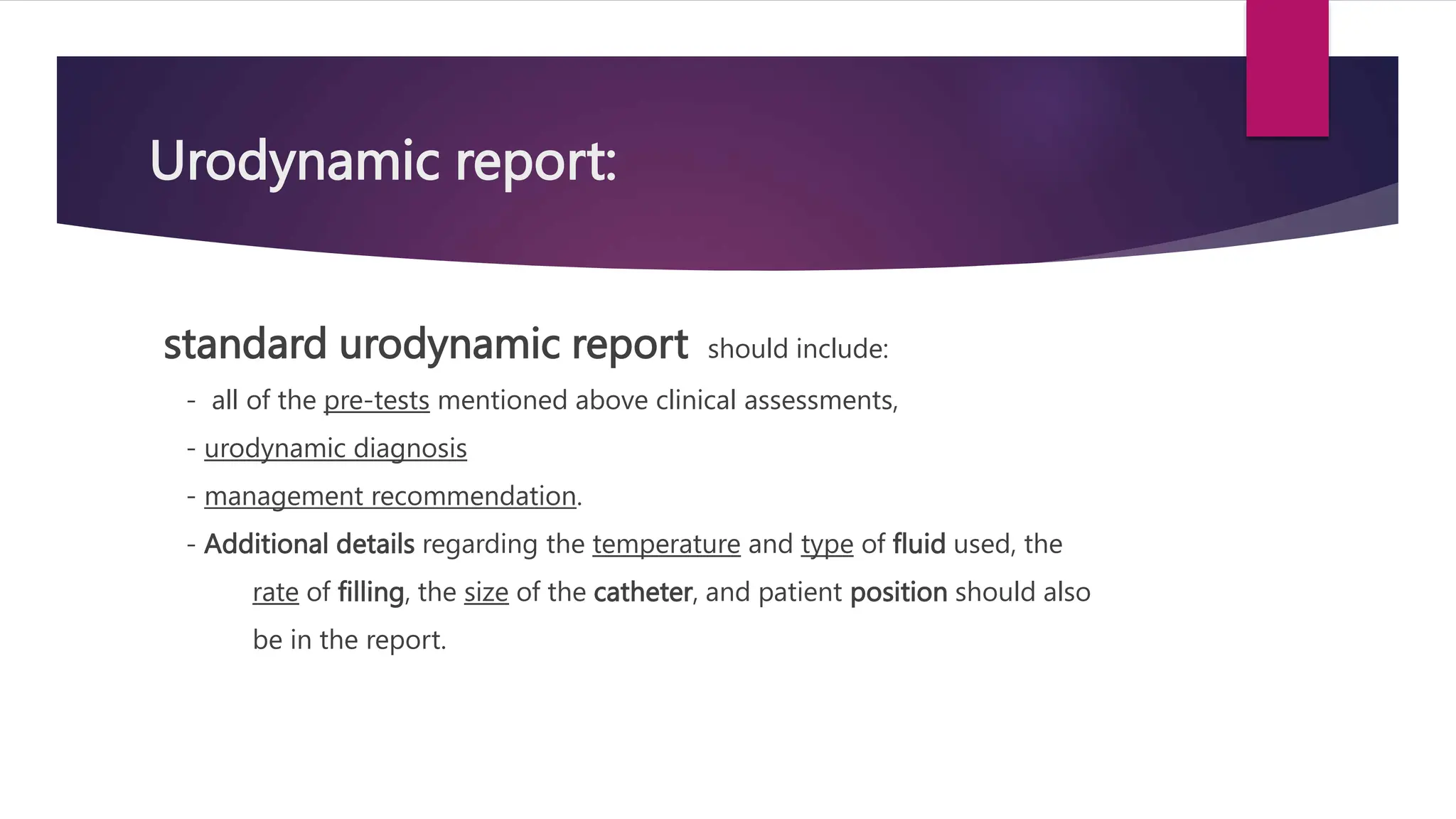
![Filling cystometry (CMG): Procedure:
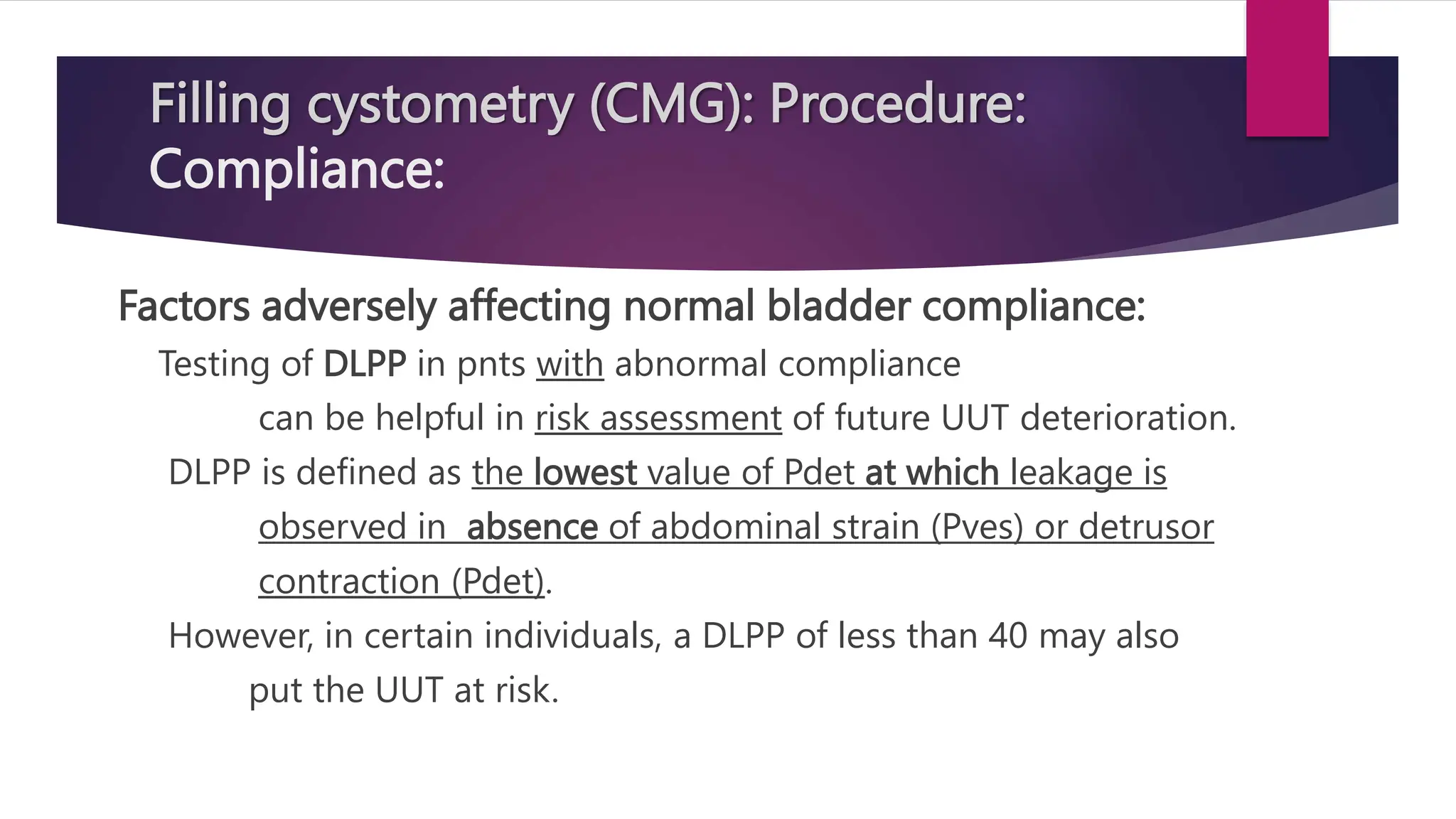
Detrusor Leak Point Pressure ( DLPP ):[ prev.bl. LPP ]
Defined by ICS as:
The lowest value of Pdet at which leakage is observed in
absence of Pabd or det. contraction.
High DLPP > 40 cm H2O may put pnts at risk for UUT
deterioration, or 2ry bl. damage in cases with neurological
dis. such as paraplegia, MS or children with MMC.
There are no data on any correlation between Det. LPP
and UUT damage in non-neurogenic pnts.](https://image.slidesharecdn.com/urodynamicstudies-231212121037-ac38053d/75/Urodynamic-studies-overview-and-examples-pptx-138-2048.jpg)
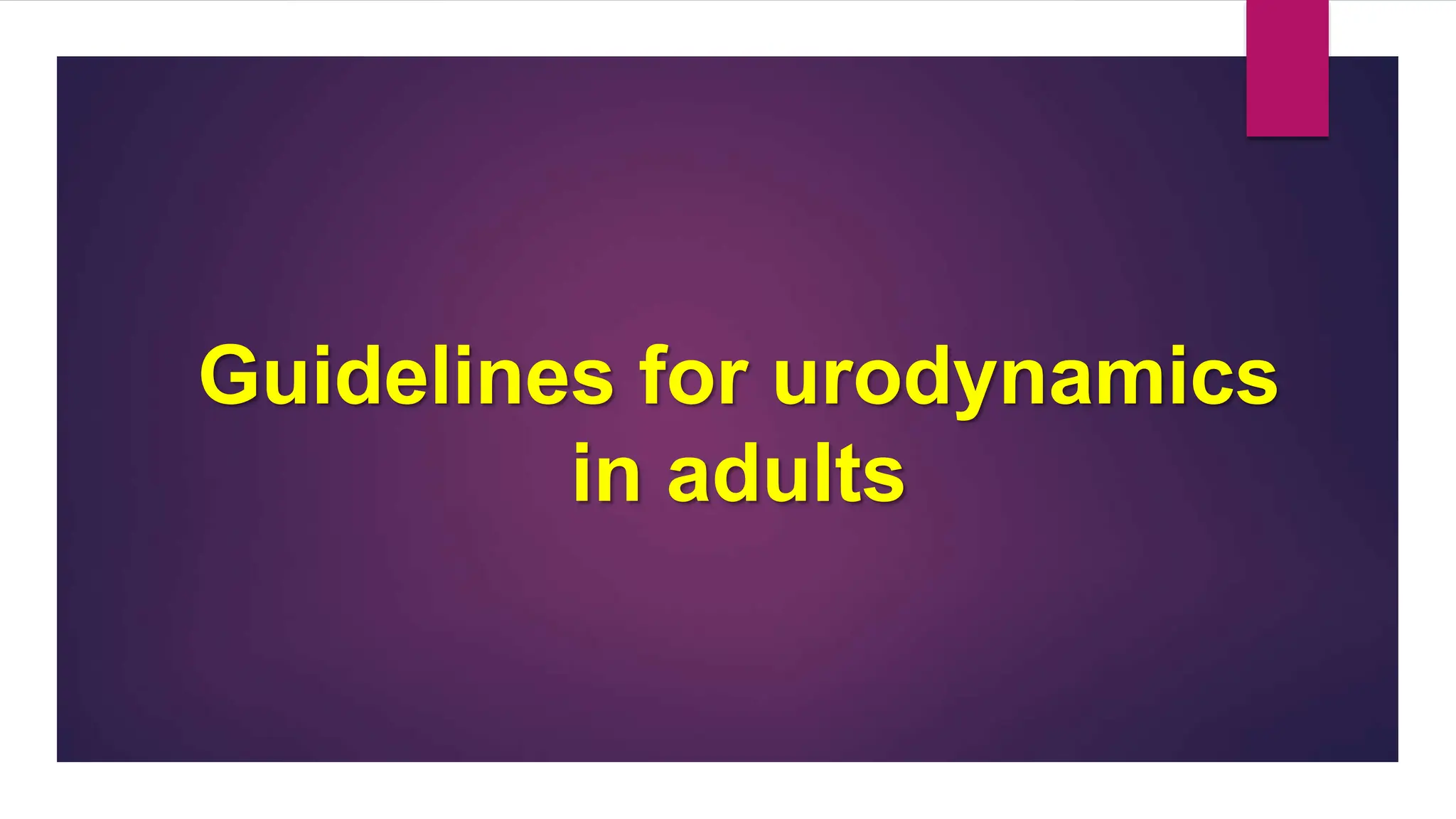
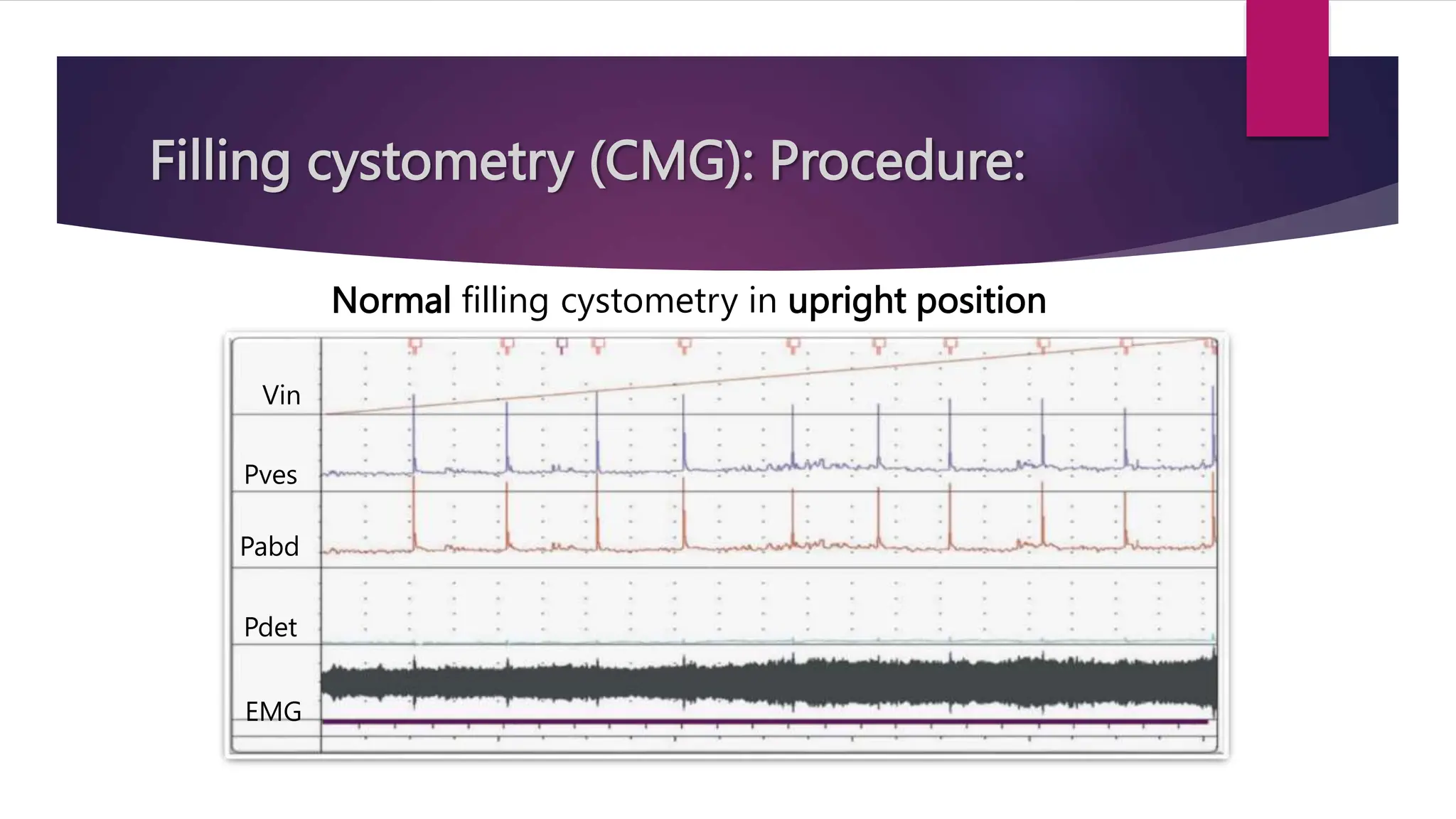
![Filling cystometry (CMG): Procedure:
Detrusor Leak Point Pressure ( DLPP ):[ prev.bl. LPP ]
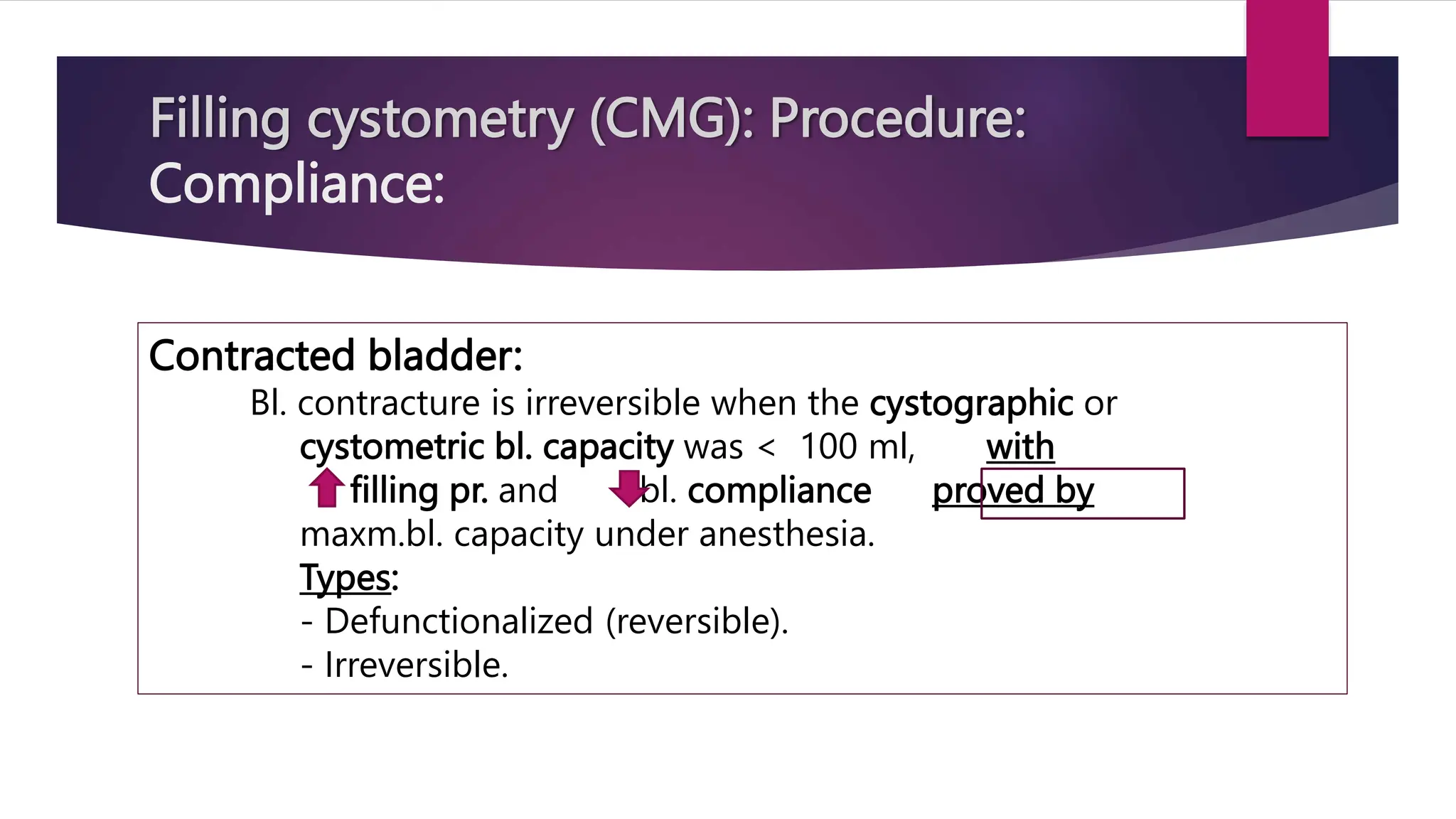
The main determinant of a normal low Pdet, during filling:
- Bl.compliance which in turn is dependent on:
- Viscoelastic properties of detrusor m.,
- Normal bl.wall composition, and
- Normal neural mechanisms.](https://image.slidesharecdn.com/urodynamicstudies-231212121037-ac38053d/75/Urodynamic-studies-overview-and-examples-pptx-139-2048.jpg)
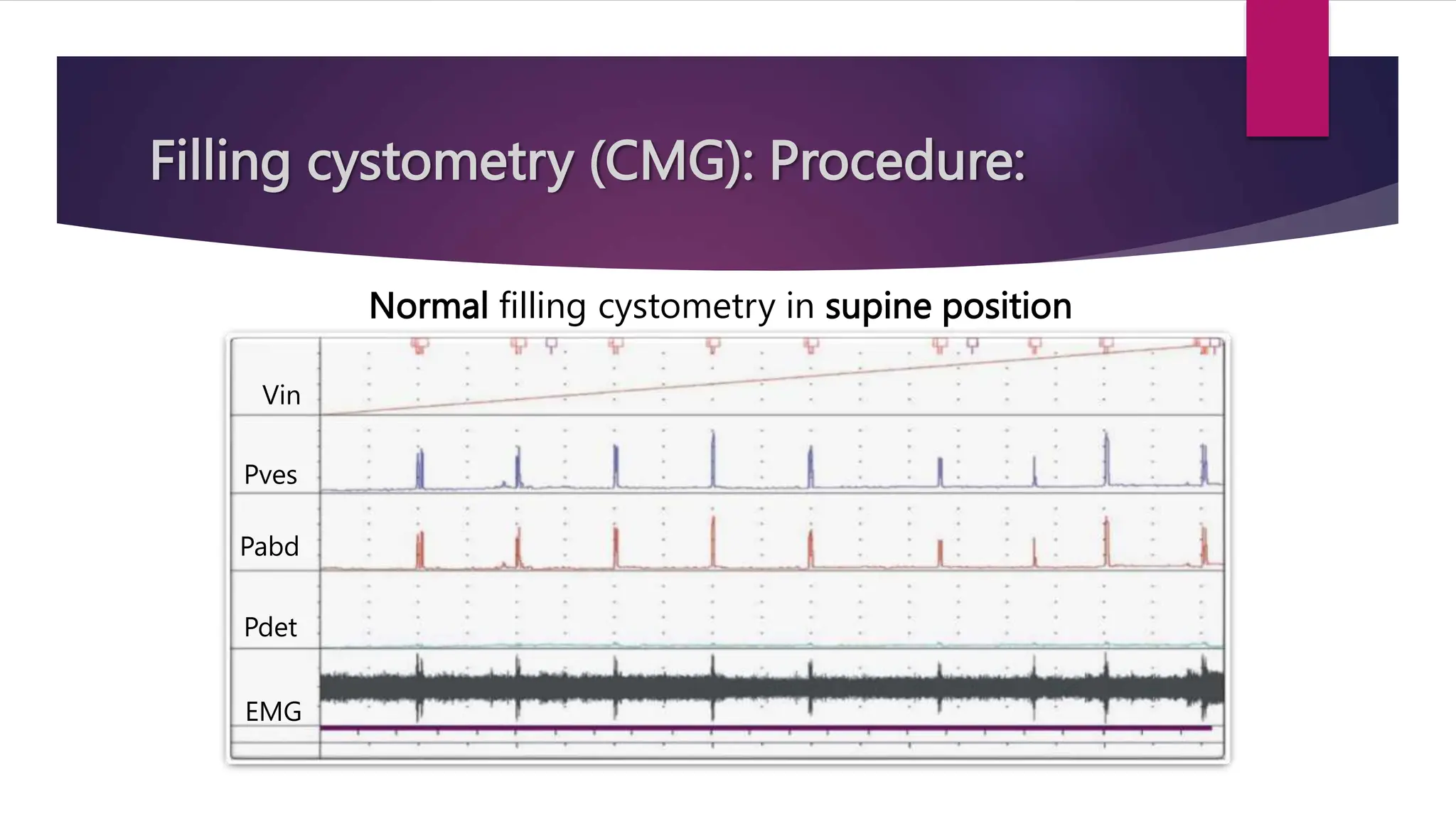
![Filling cystometry (CMG): Procedure:
Detrusor Leak Point Pressure ( DLPP ):[ bladder LPP ]
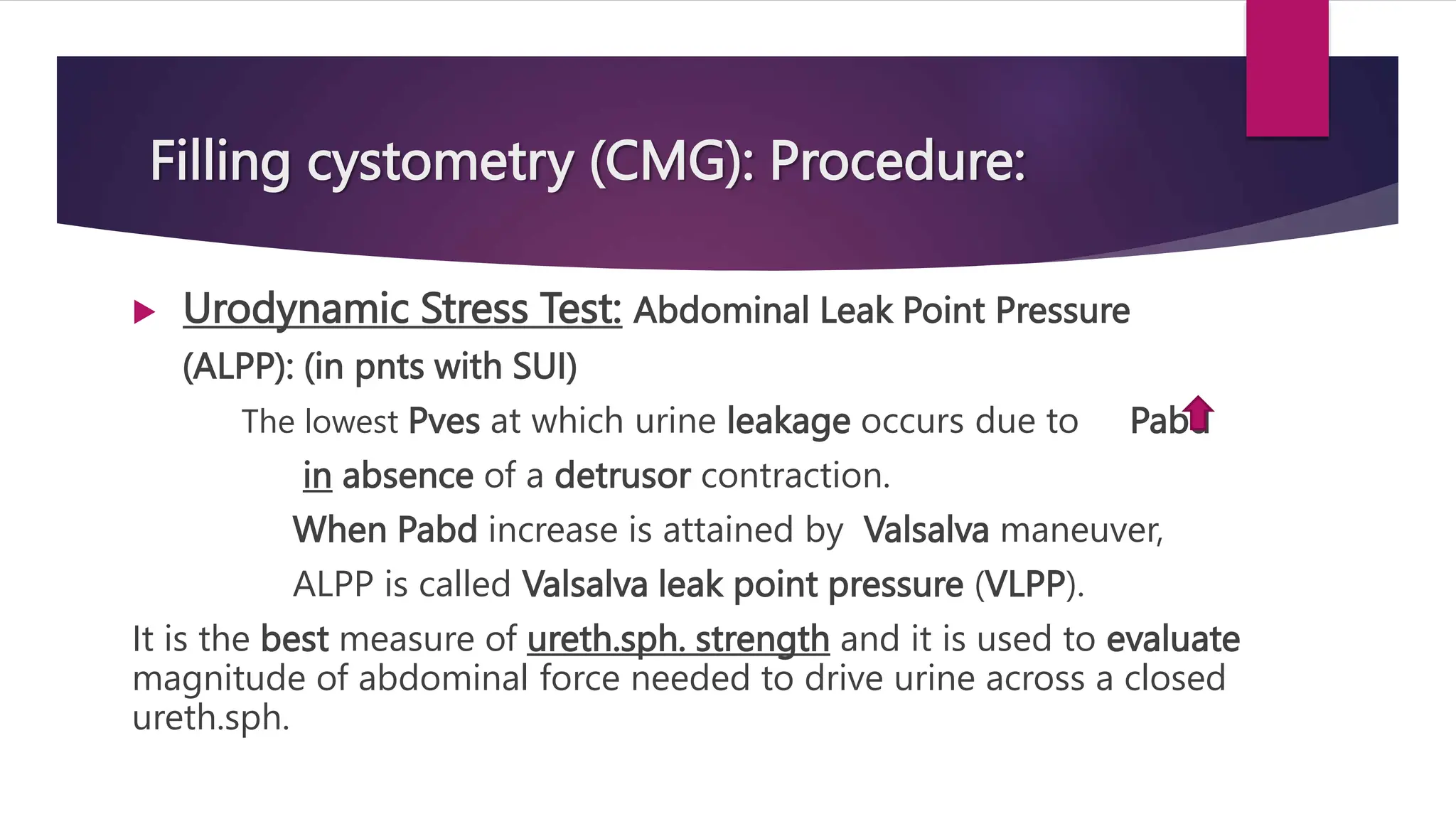
In neurogenic bladder, DLPP > 40 cmH2O is considered as high-risk
factor for upper urinary tract deterioration.
Detrusor overactivity leak point pressure (DOLPP):
lowest Pdet with DO at which urine leakage first occurs in the
absence of voluntary detrusor contraction or Pabd.](https://image.slidesharecdn.com/urodynamicstudies-231212121037-ac38053d/75/Urodynamic-studies-overview-and-examples-pptx-140-2048.jpg)
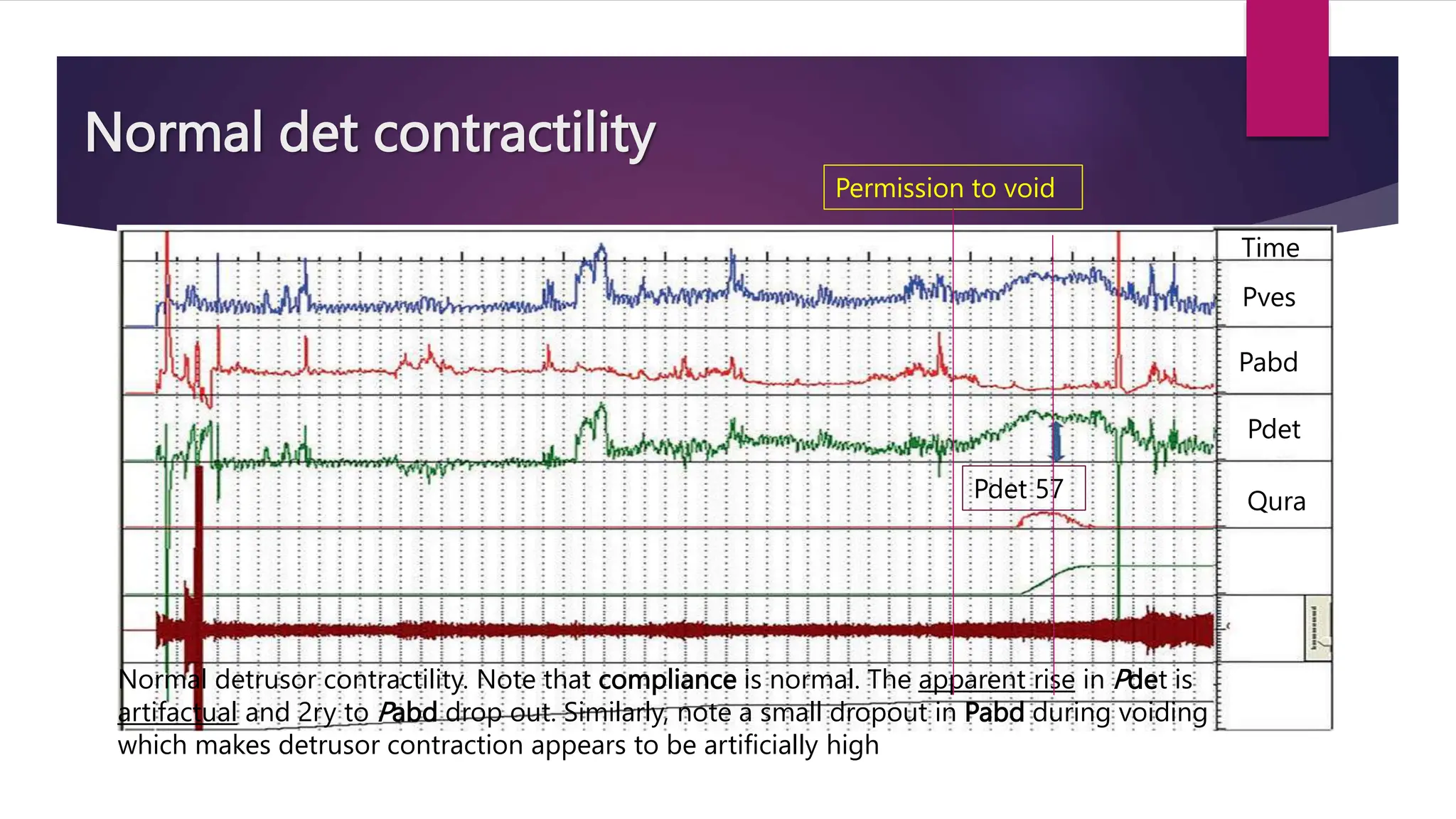
![Filling cystometry (CMG): Procedure:
Detrusor Leak Point Pressure ( DLPP ):[ bladder LPP ]
Detrusor leak point volume (DLPV):
Bladder volume at which first urine leakage occurs,
either with DO or low compliance.](https://image.slidesharecdn.com/urodynamicstudies-231212121037-ac38053d/75/Urodynamic-studies-overview-and-examples-pptx-141-2048.jpg)
![Filling cystometry (CMG): Procedure:
Detrusor Leak Point Pressure
( DLPP ):[ bladder LPP ]
DLPP > 40 cmH2O in pnt
with long-term chronic stage of
cauda equine syndrome with
bilateral chronic poly-
radiculopathy below L5 level.](https://image.slidesharecdn.com/urodynamicstudies-231212121037-ac38053d/75/Urodynamic-studies-overview-and-examples-pptx-142-2048.jpg)