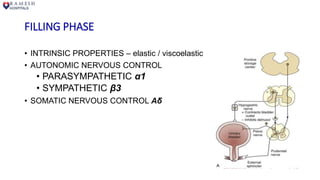
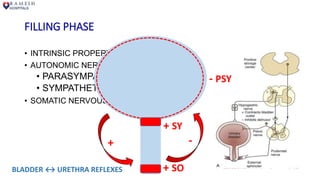
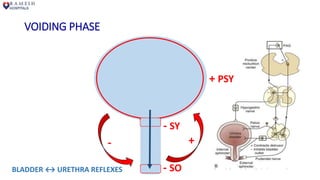
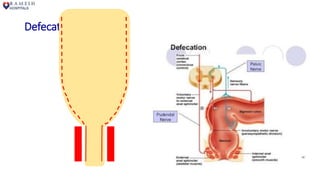
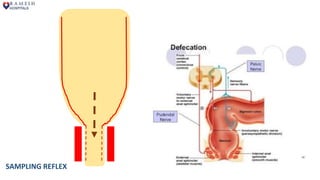
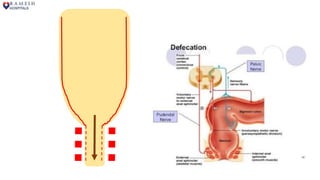
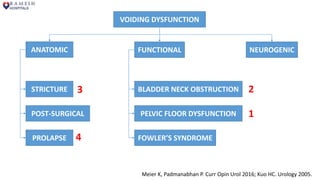
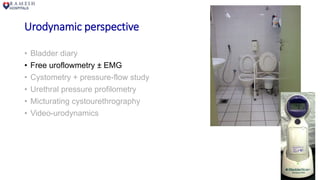
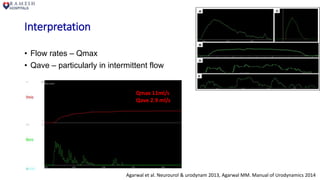
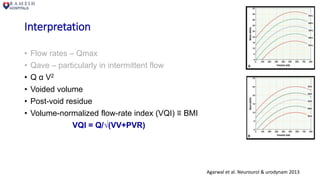
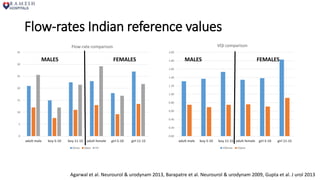
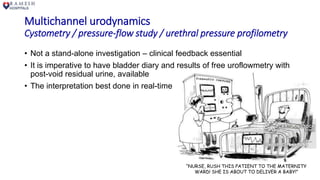
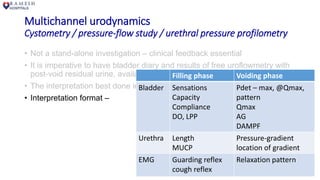
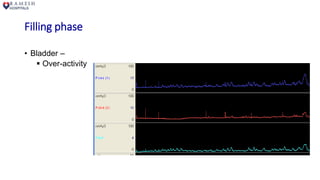
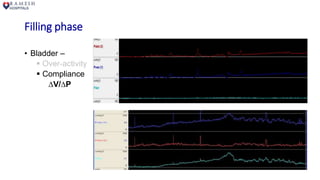
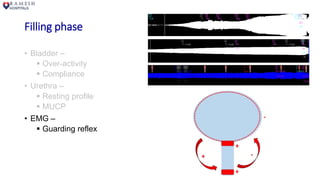
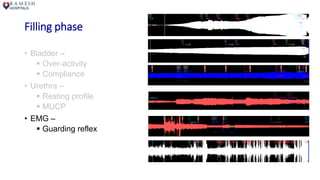
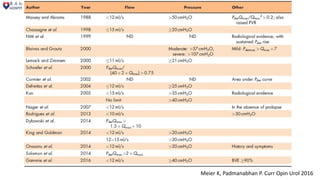
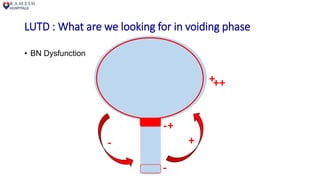
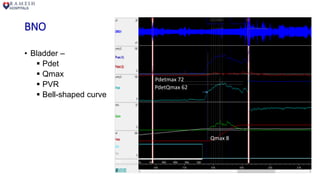
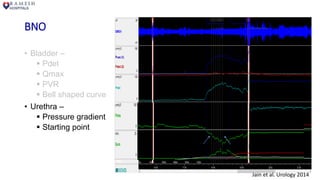
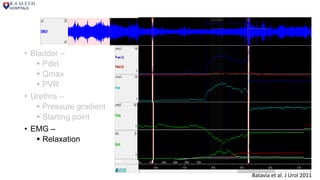
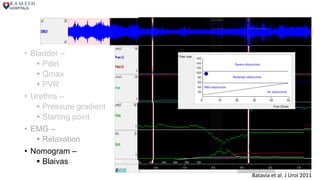
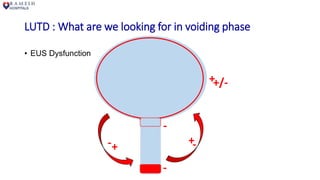
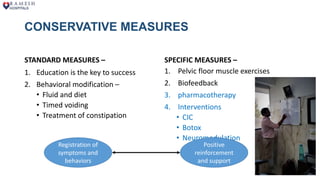
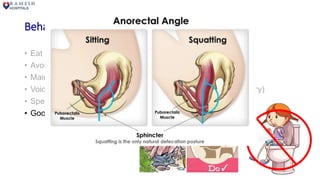
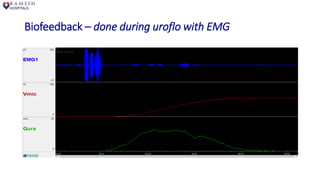
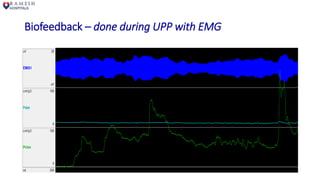
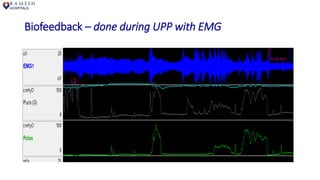
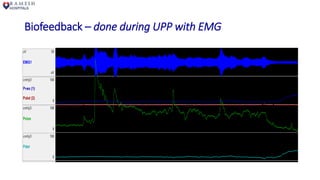
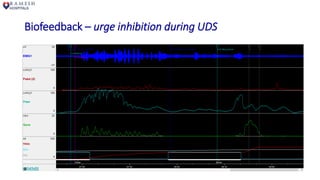
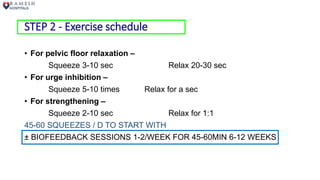
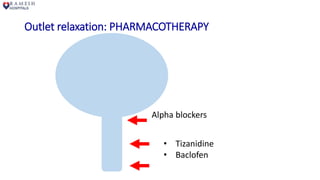
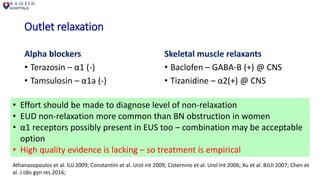
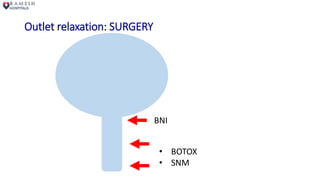
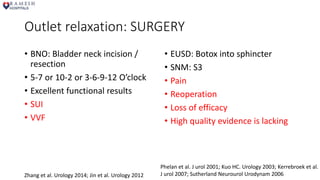
The document discusses the diagnosis and management of voiding dysfunction in women, outlining key physiological aspects of the lower urinary tract, urodynamic evaluations, and potential treatment options. It emphasizes the importance of real-time interpretation of urodynamics, behavioral modifications, and biofeedback as crucial elements in therapy. The conclusion highlights the need for a balanced approach due to the lack of high-quality evidence supporting various treatments.