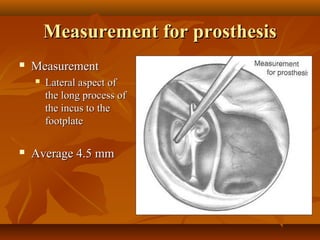
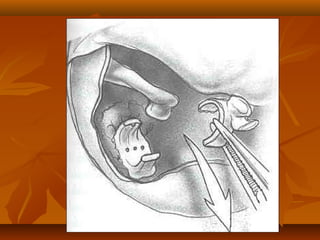
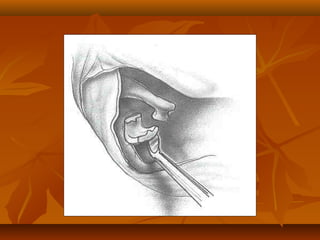
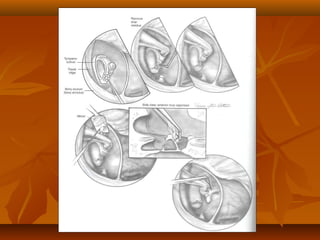
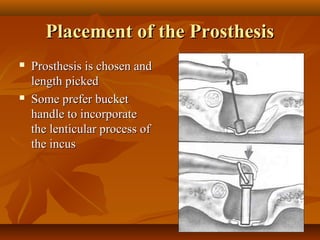
Measure and mark
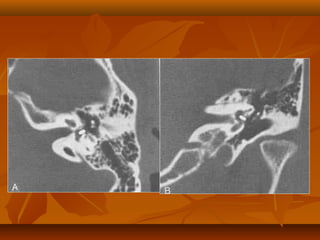
incus and oval window
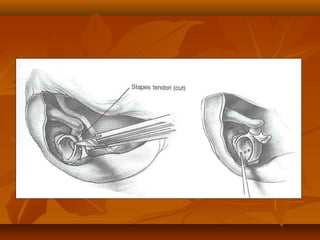
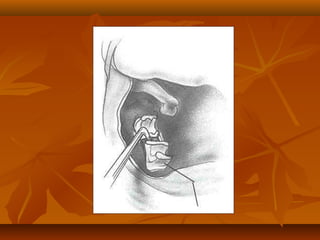
�Removal of stapes suprastructure
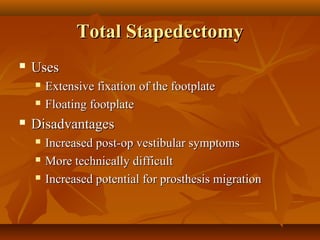
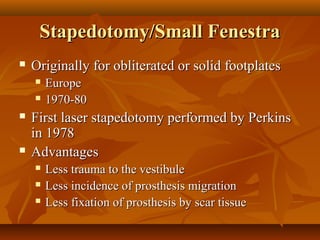
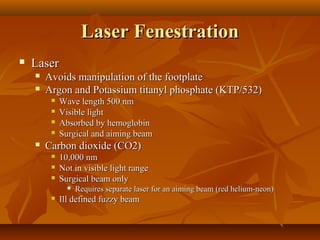
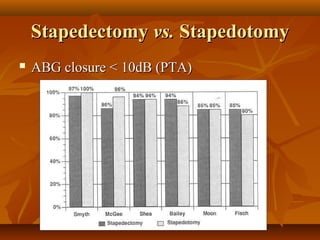
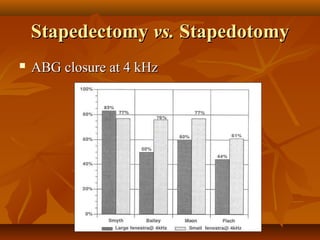
Stapedotomy vs.
stapedectomy
Drill vs. laser vs.
microscissors
Avoid injury to the
facial nerve and
cochlea
Remove all
suprastructure
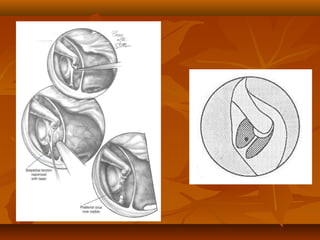
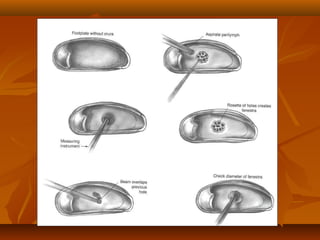
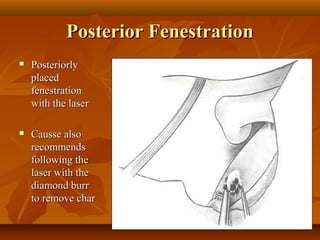
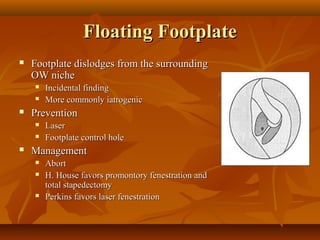
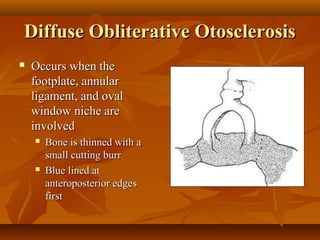
�Oval window preparation
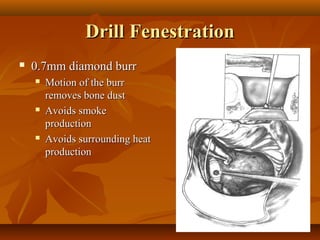
Remove any
overhanging bone
with a diamond burr
Ensure a clean
circular opening
Avoid injury to the
facial nerve and
cochlea
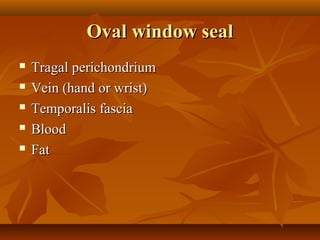
Seal any perilymph
leaks
�Pro