This document provides an overview of osteoporosis, including its definition, epidemiology, diagnosis, pathophysiology, clinical features, differential diagnosis, outcome measures, management, and more. Some key points:
- Osteoporosis is defined as a systemic skeletal disease characterized by low bone mass and deterioration of bone tissue, leading to fragile bones and increased susceptibility to fractures.
- It predominantly affects postmenopausal women, with prevalence as high as 80% in India having osteoporosis or osteopenia.
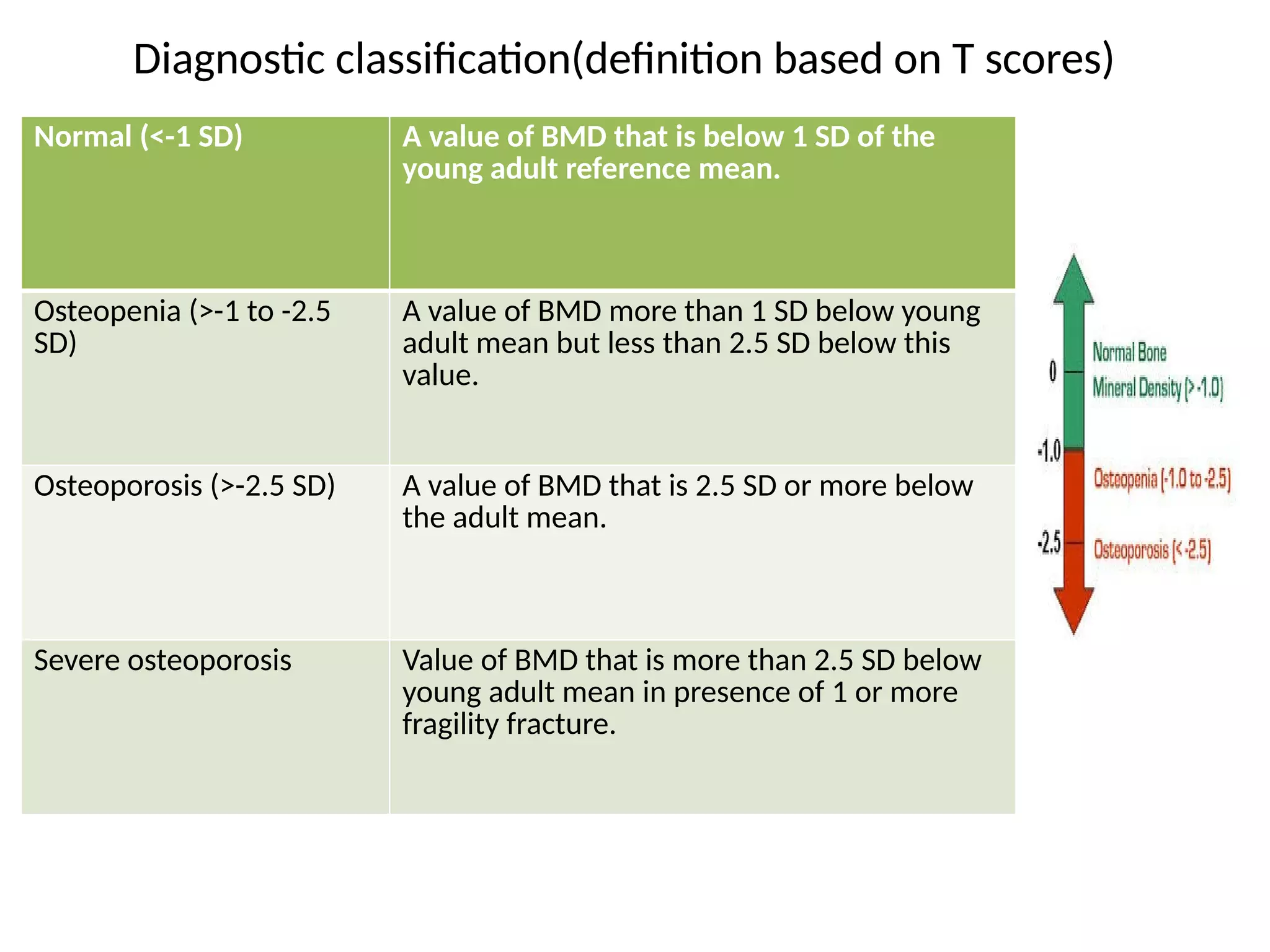
- Diagnosis is based on bone mineral density T-scores measured via dual-energy x-ray absorptiometry. Medical management involves antiresorptive and an