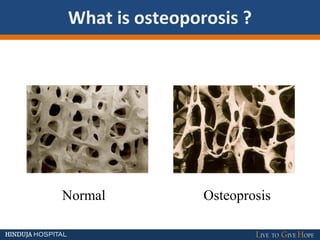
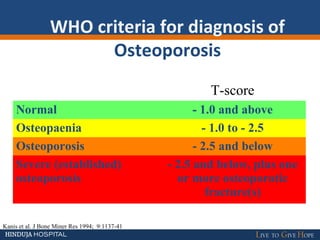
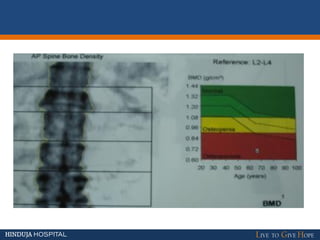
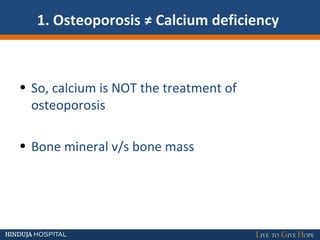
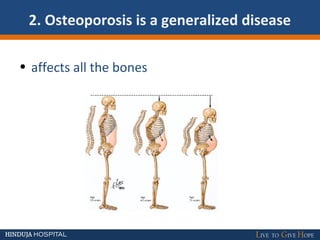
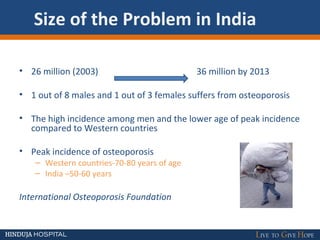
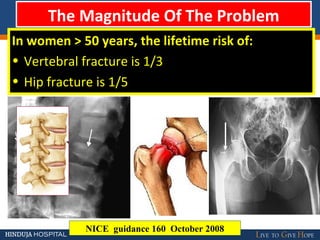
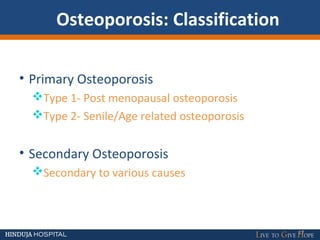
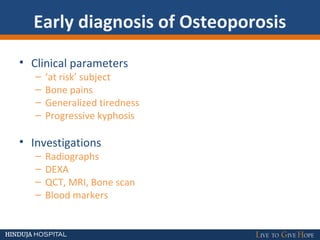
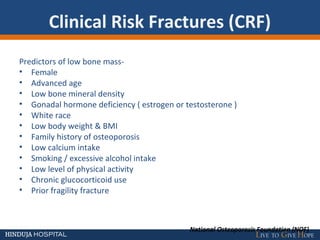
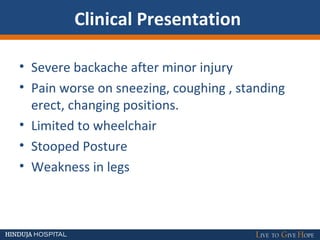
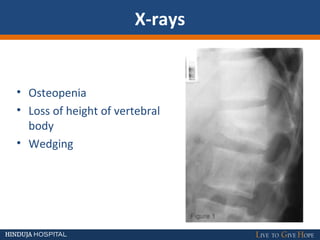
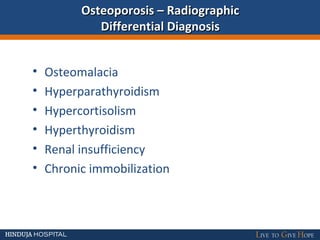
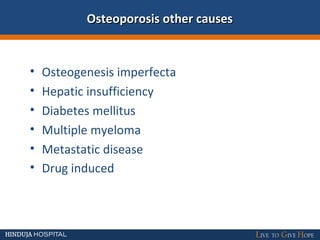
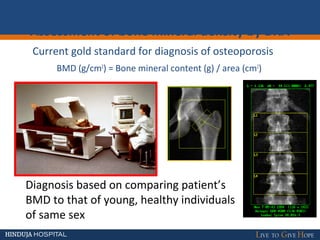
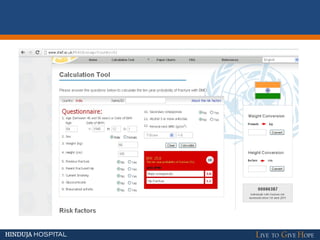
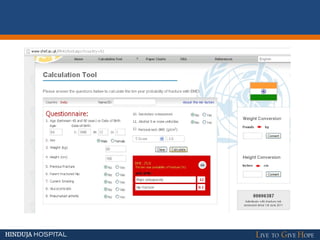
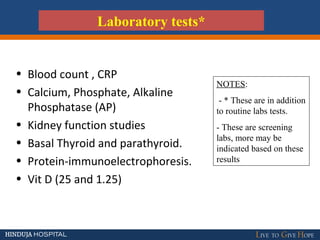
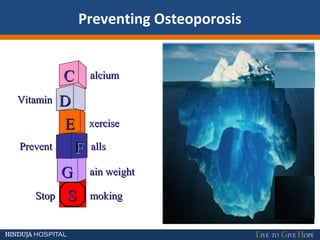
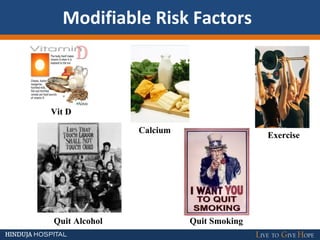
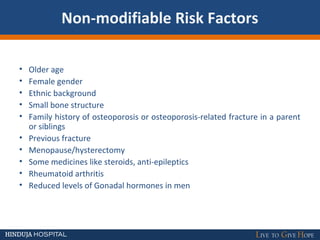
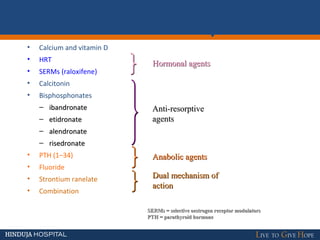
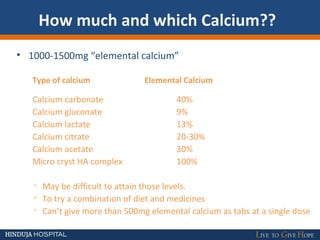
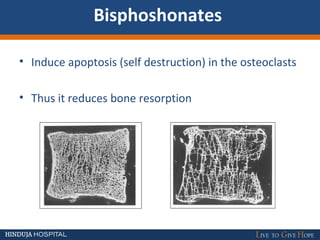
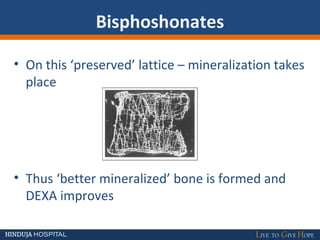
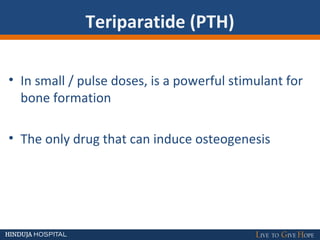
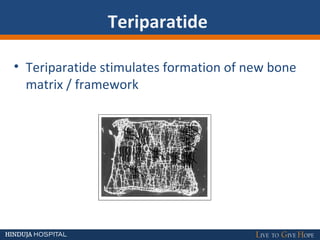
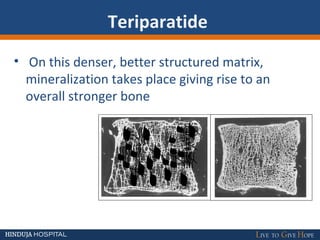
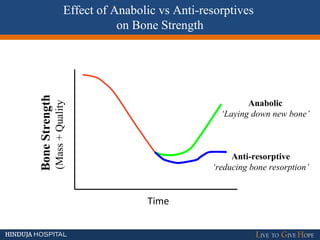
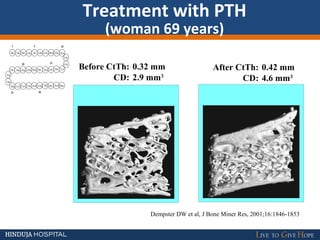
The document discusses osteoporosis, a condition characterized by the softening and reduction of bone quality, significantly affecting older individuals, particularly women over 50. It outlines the diagnosis criteria, risk factors, and the importance of early detection and prevention, highlighting the prevalence of osteoporosis in India. Treatment options include lifestyle changes, calcium and vitamin D supplementation, and medications such as bisphosphonates.