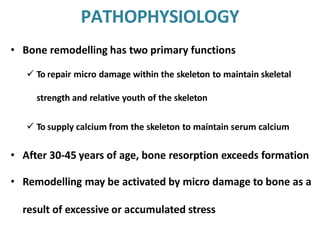
Osteoporosis is a disease characterized by low bone mass and structural deterioration of bone tissue, leading to bone fragility and an increased risk of fractures. Key points:
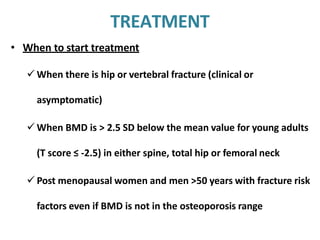
- It is defined as a bone density 2.5 standard deviations or more below the mean bone density of healthy young adults.
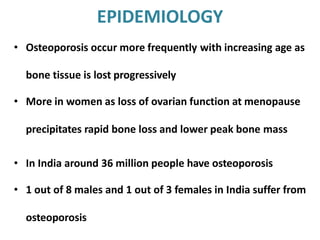
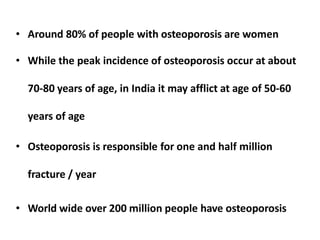
- It occurs more frequently with age and is more common in women, especially after menopause due to estrogen loss.
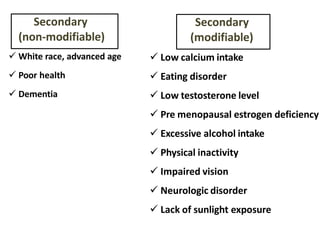
- Risk factors include family history, smoking, low weight, inactivity, excessive alcohol, and certain medical conditions or medications.
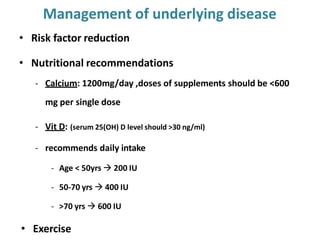
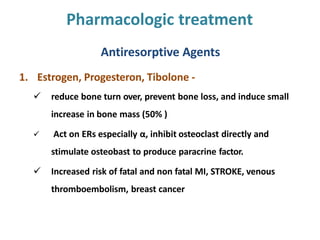
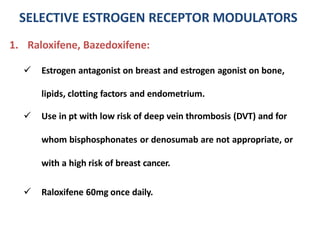
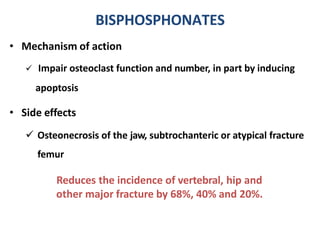
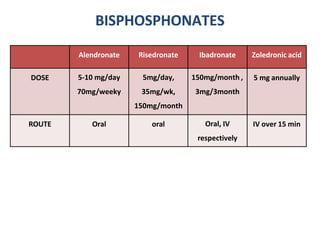
- It is usually asymptomatic until a fracture occurs. Treatment focuses on lifestyle changes, calcium/vitamin D supplementation, and medications to increase bone density