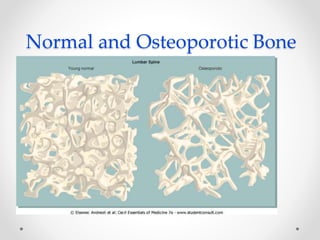
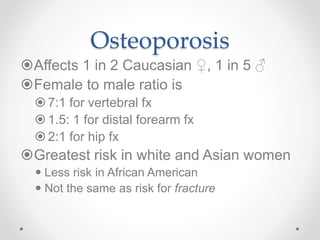
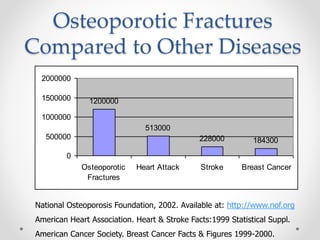
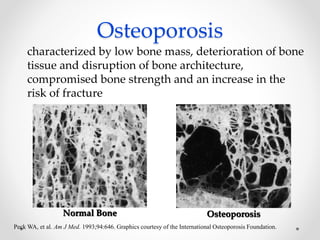
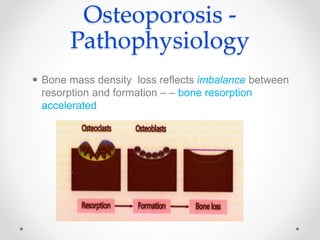
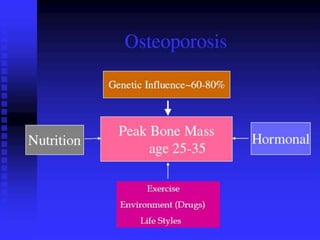
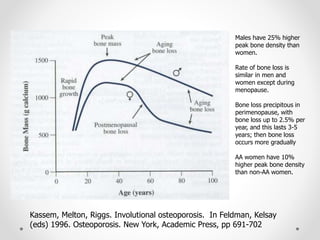
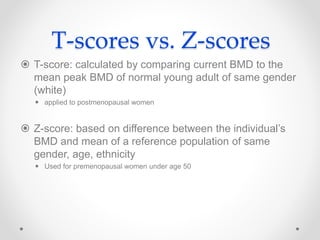
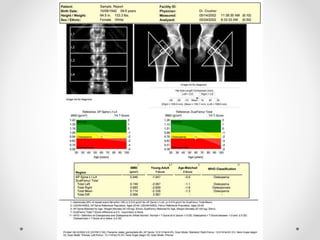
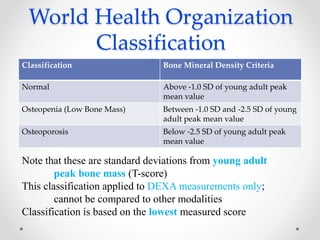
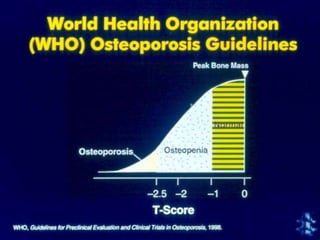
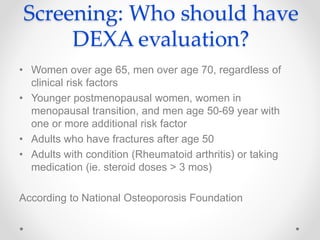
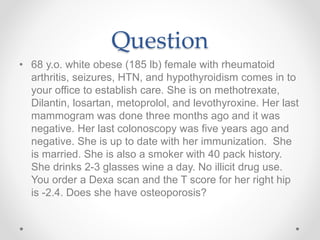
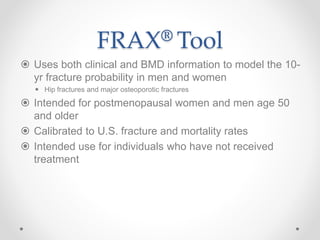
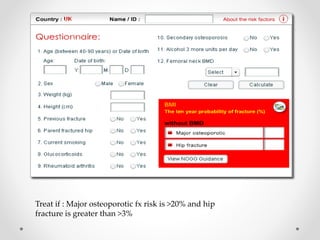
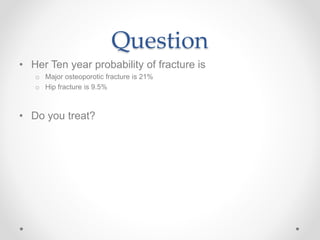
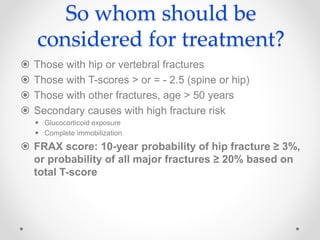
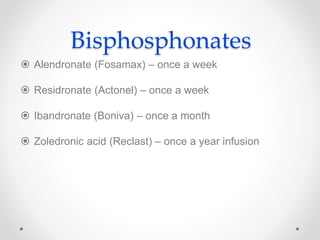
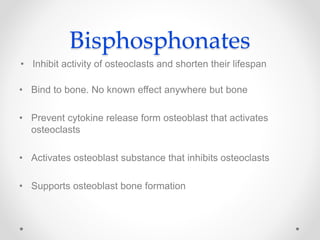
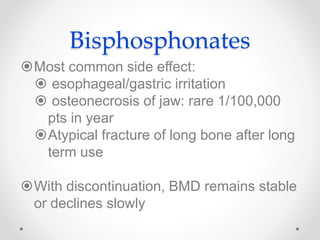
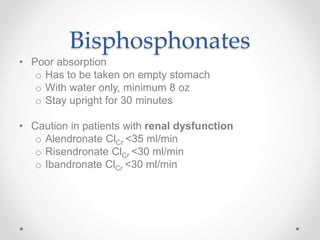
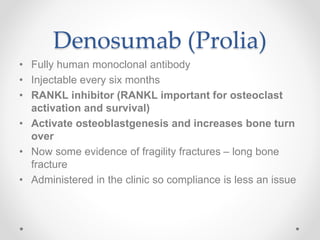
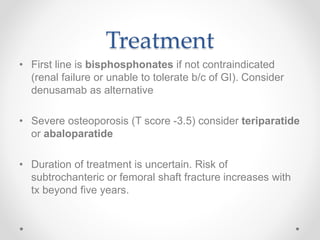
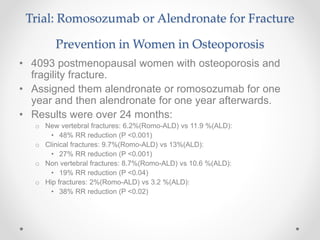
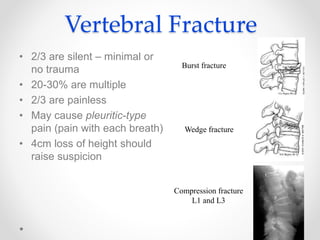
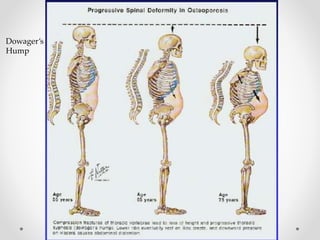
Osteoporosis is a prevalent bone disorder characterized by compromised bone strength and an increased risk of fractures, affecting 40 million people globally, particularly postmenopausal women. The condition arises from an imbalance in bone remodeling, primarily accelerated during menopause, and is diagnosed using dual-energy x-ray absorptiometry (DEXA) scans which measure bone mineral density. Treatment options include bisphosphonates, antiresorptives, and anabolic agents, with patients being screened based on age and clinical risk factors.