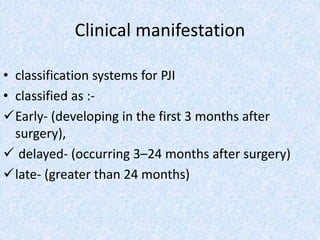
The document discusses osteomyelitis, an infection of bone and bone marrow, and prosthetic joint infection, detailing definitions, etiological agents, clinical manifestations, laboratory diagnoses, and treatment approaches. Osteomyelitis is primarily caused by bacteria and affects mainly children, while prosthetic joint infections can arise from direct inoculation or hematogenous seeding, with various treatment strategies including surgical options and antibiotic therapy. The document cites several references for further reading on these medical topics.