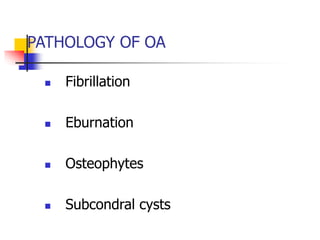
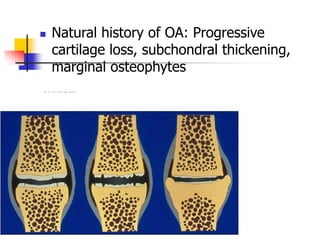
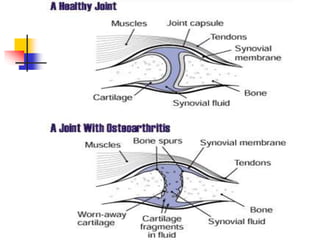
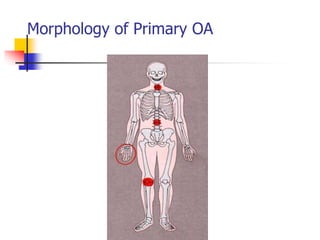
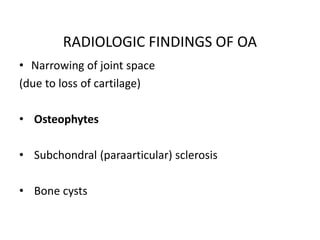
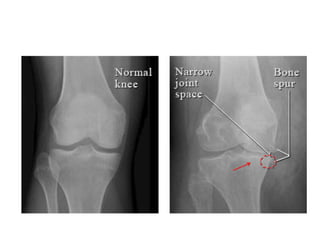
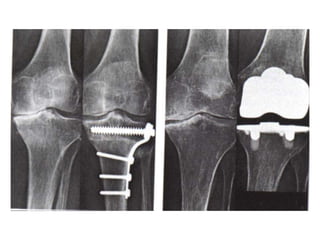
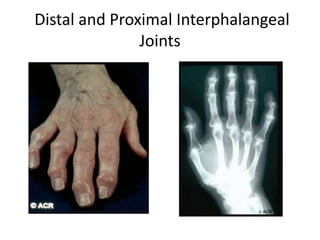
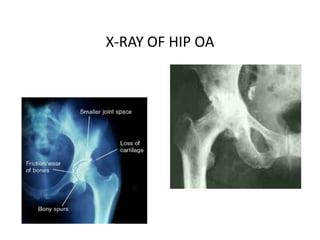
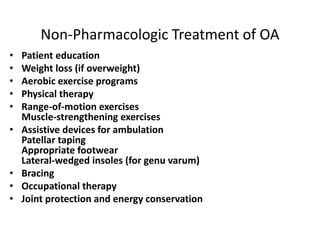
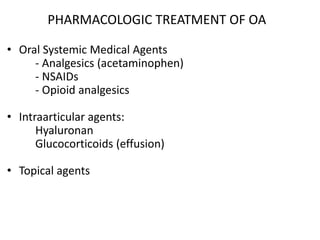
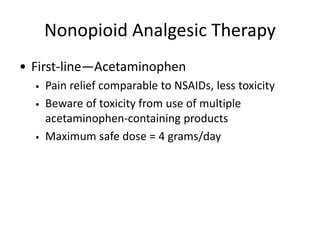
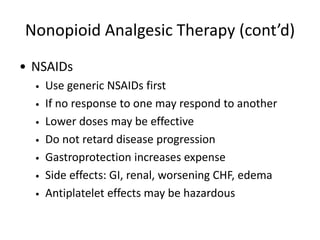
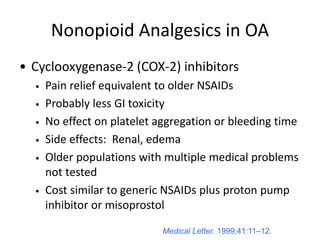
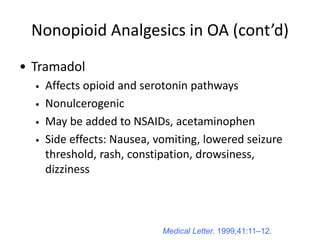
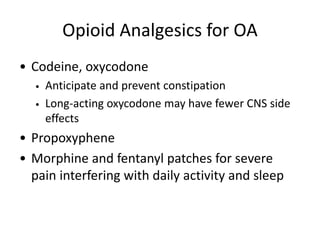
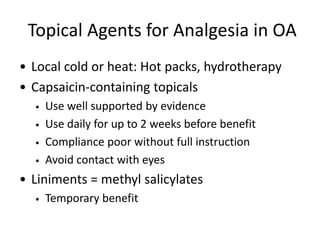
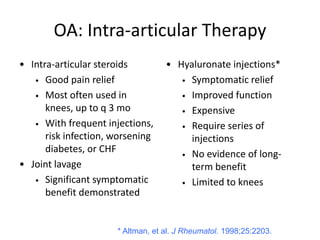
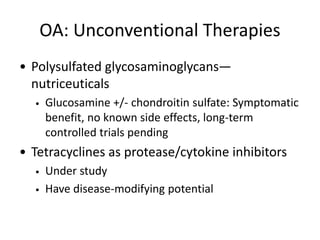
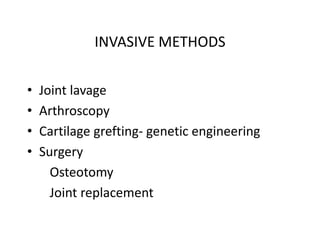
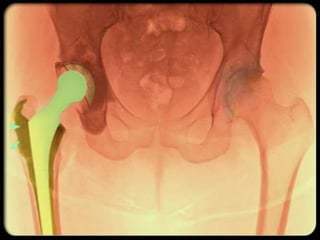
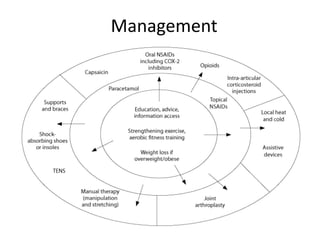
Osteoarthritis is a degenerative joint disease characterized by cartilage breakdown. It is the most common form of arthritis, often affecting the knees in 70% of people over age 60. Osteoarthritis can cause functional impairment and disability in older adults and is a leading cause of joint replacement surgery. Risk factors include age, obesity, genetics, and joint trauma. Treatment focuses on reducing pain and preserving function through lifestyle changes, physical therapy, braces, and medications like acetaminophen, NSAIDs, and opioids. Surgery is considered for severe, treatment-resistant cases.