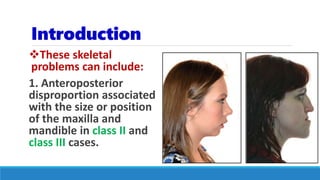
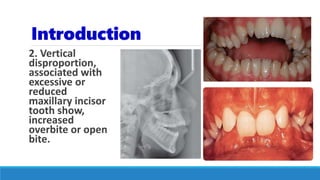
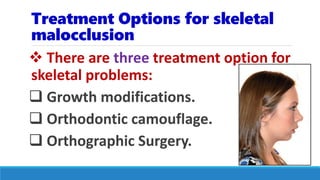
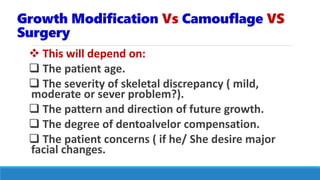
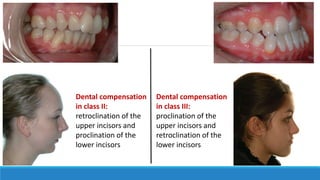
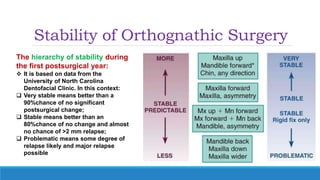
1. The document discusses treatment options for skeletal malocclusions, including growth modification, orthodontic camouflage, and orthognathic surgery.
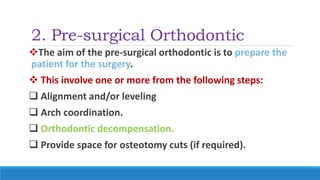
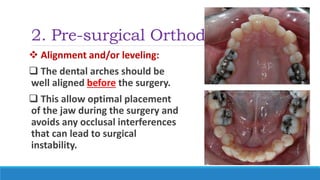
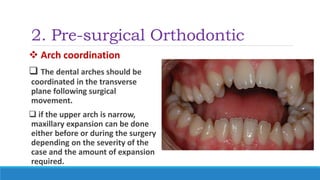
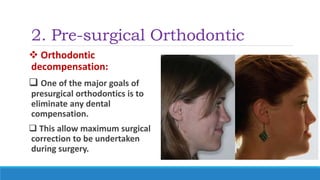
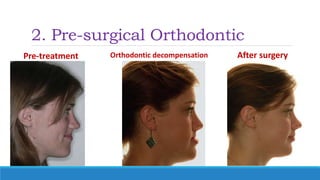
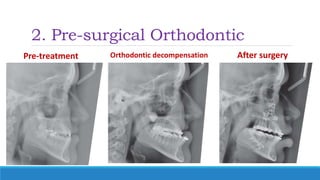
2. Pre-surgical orthodontic treatment aims to prepare the patient for surgery through procedures like alignment, decompensation, and creating space for osteotomies.
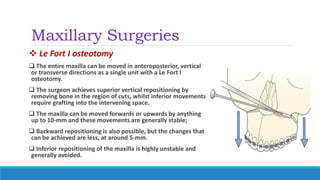
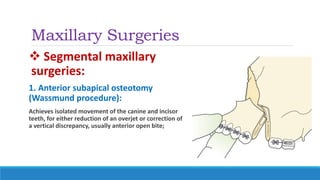
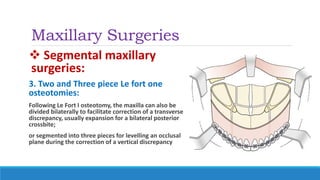
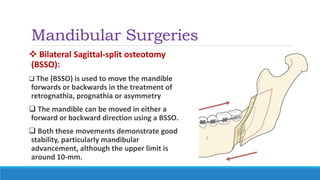
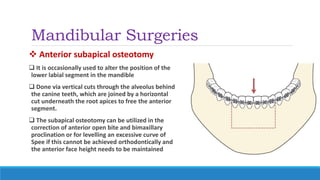
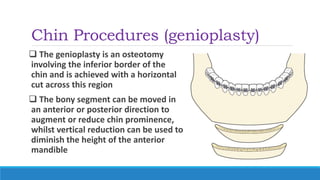
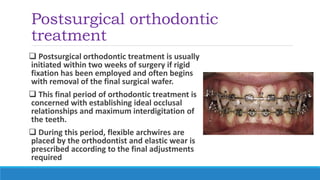
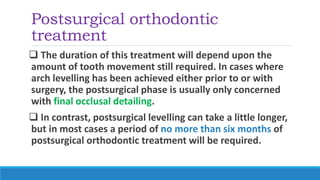
3. Surgical procedures discussed include Le Fort I osteotomy for the maxilla, bilateral sagittal split osteotomy for the mandible, and genioplasty for the chin. Post-surgical orthodontics establishes the final occlusion.