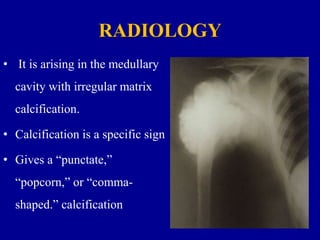
This document discusses chondrosarcoma, a type of bone cancer. It is a malignant tumor originating from cartilage that makes up 9% of primary bone cancers. The document covers the classification, most common sites in the body, clinical features, diagnosis using imaging like CT and MRI, histological examination, treatment including wide resection or amputation, and prognosis which depends on grade and size of the tumor. Chondrosarcoma can be primary, arising directly in bone, or secondary from pre-existing benign cartilage lesions. Low-grade lesions have over 90% 10-year survival while high-grade have 20-40% 10-year survival.