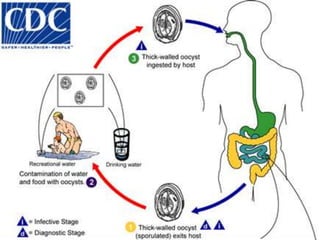
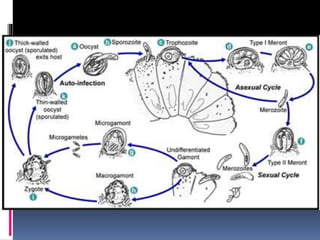
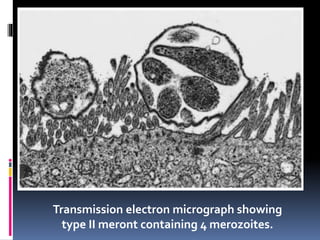
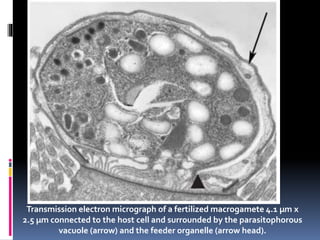
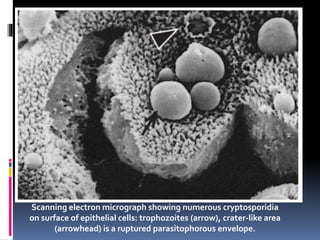
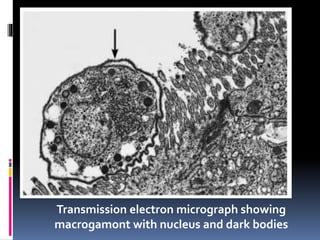
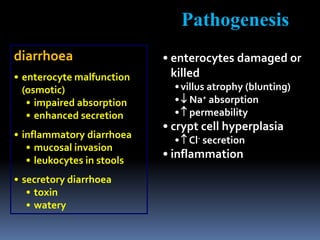
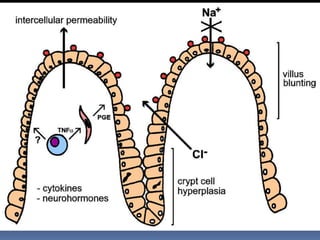
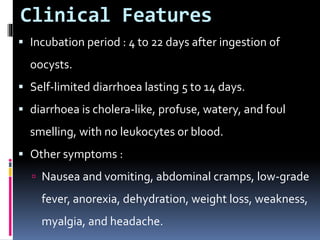
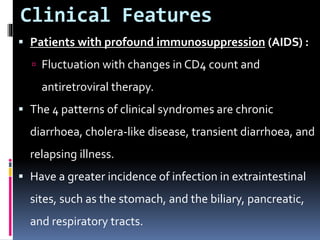
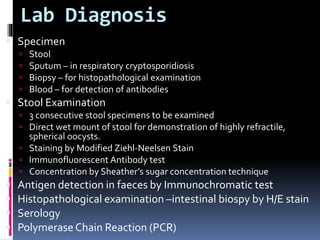
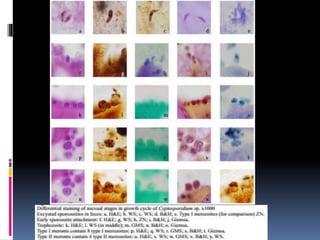
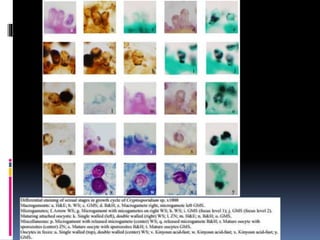
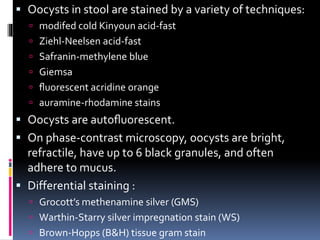
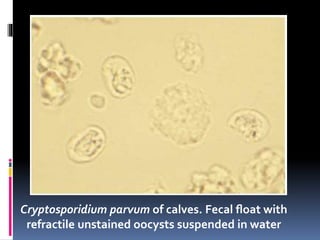
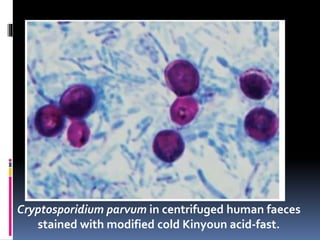
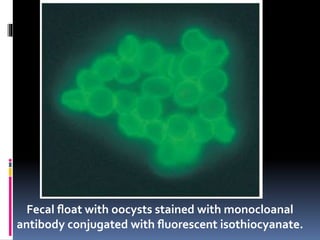
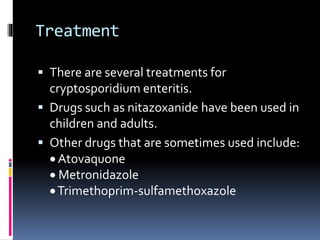
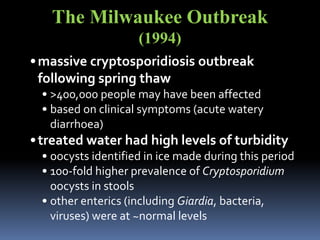
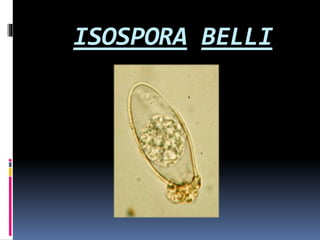
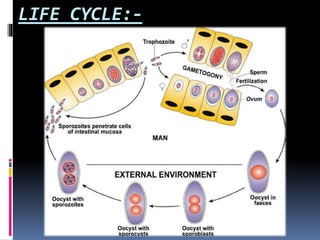
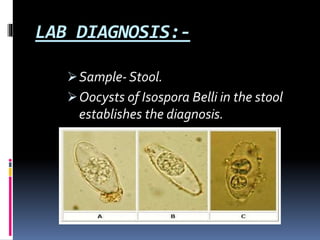
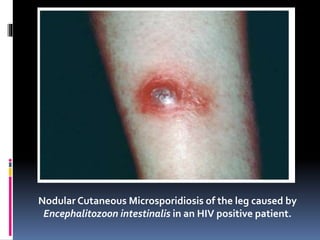
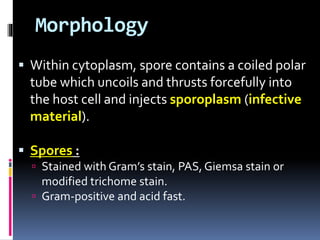
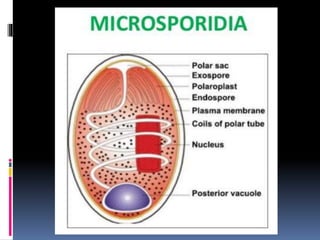
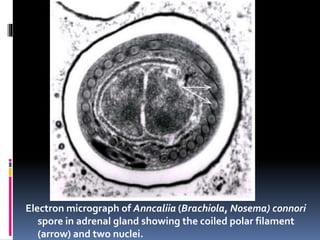
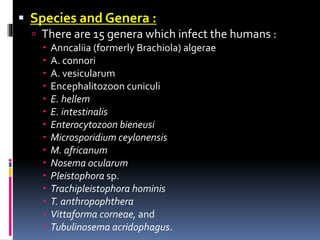
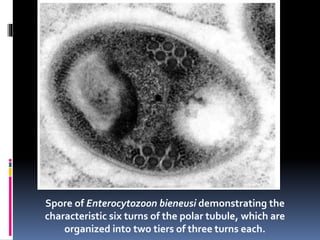
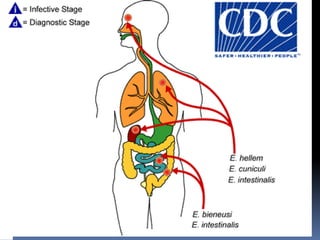
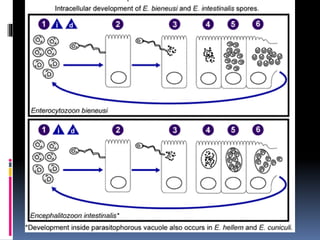
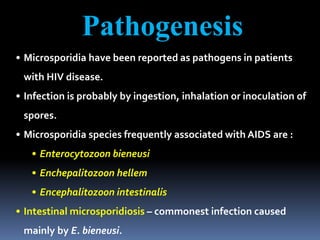
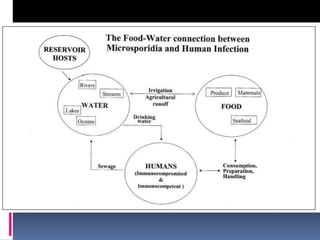
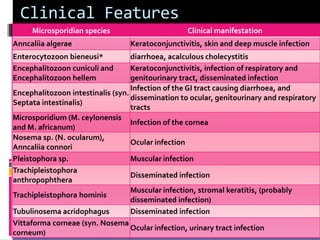
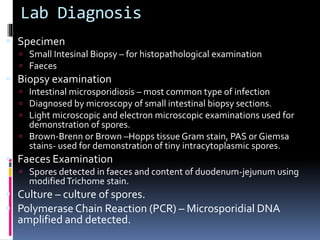
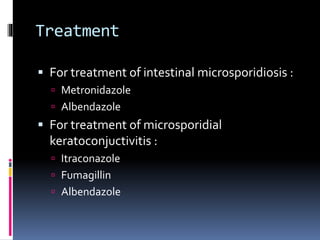
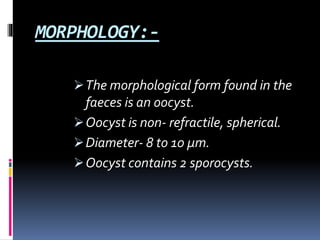
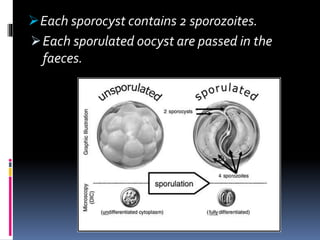
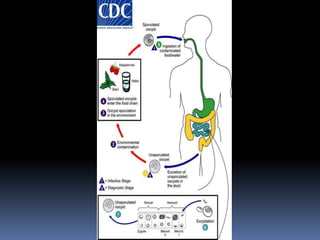
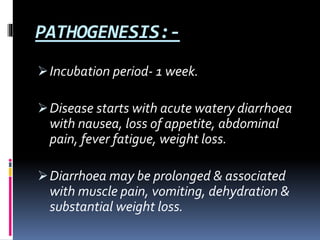
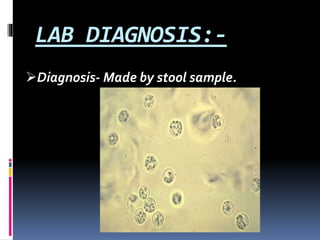
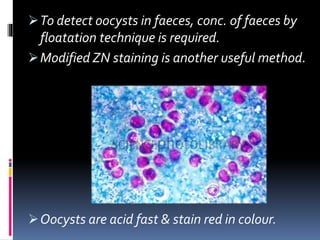
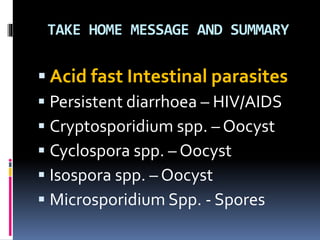
This document discusses various opportunistic protozoans that can cause disease in humans, including Cryptosporidium, Microsporidia, Cyclospora, and Isospora. It provides details on the morphology, life cycles, transmission, clinical symptoms, and laboratory diagnosis of Cryptosporidium parvum and Isospora belli. It also discusses an outbreak of cryptosporidiosis in Milwaukee in 1994 and various human pathogens within the phylum Microspora.