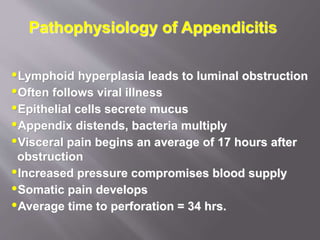
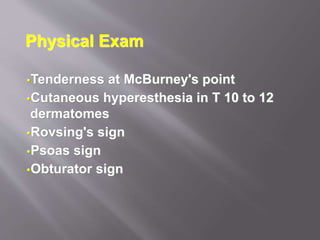
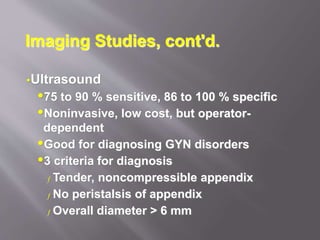
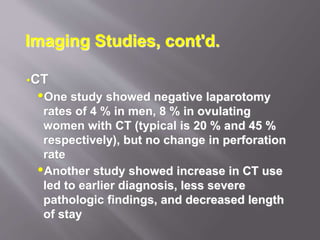
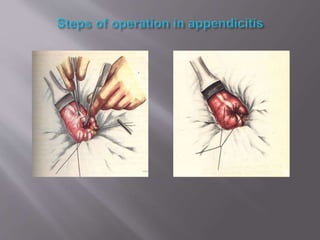
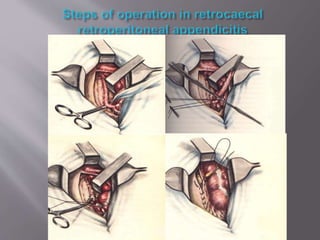
This document outlines the anatomy, pathophysiology, diagnostic considerations, and management of appendicitis, emphasizing common presentations and risk factors. It discusses imaging studies, laboratory evaluations, and differential diagnoses, providing a detailed overview for effective diagnosis and treatment. Surgical procedures for appendectomy are described step-by-step, highlighting techniques and considerations for various patient populations.