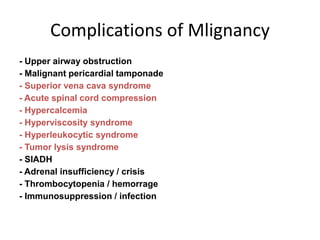
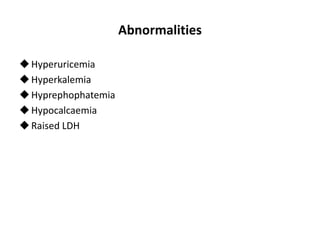
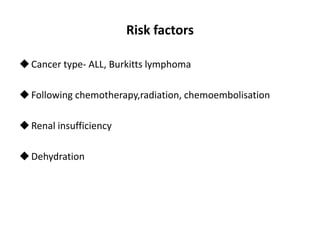
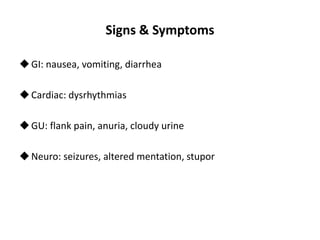
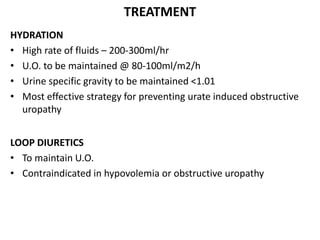
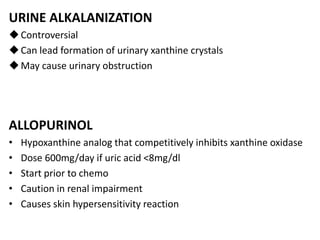
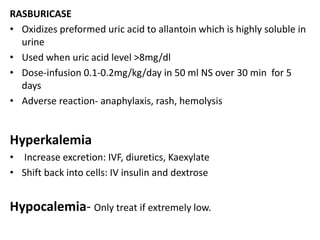
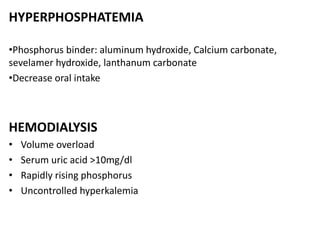
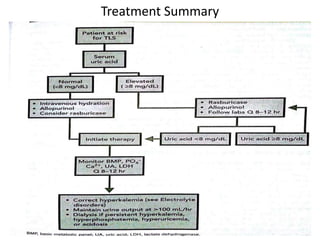
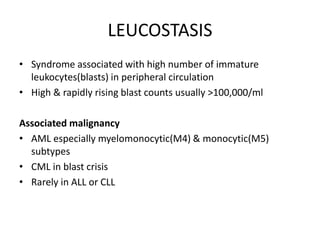
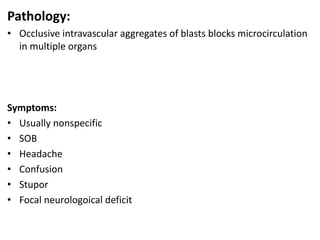
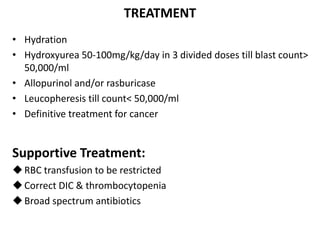
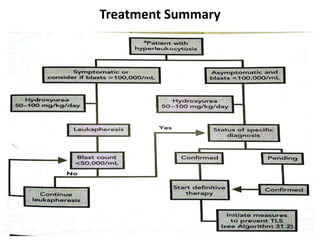
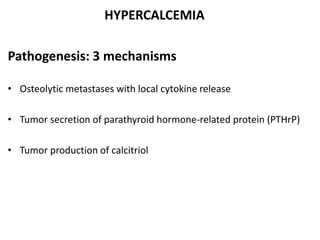
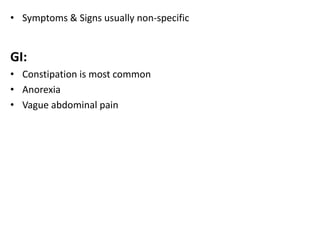
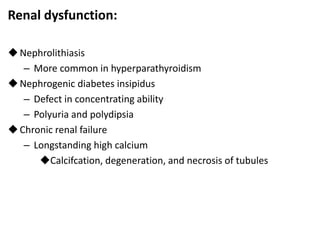
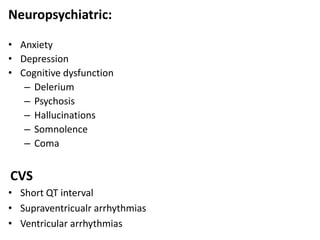
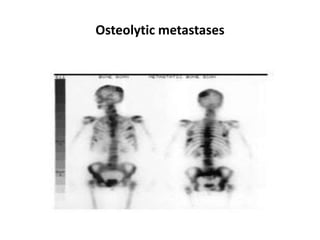
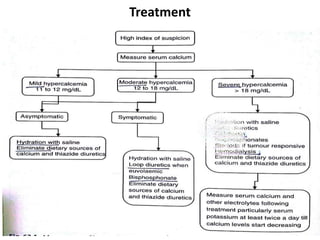
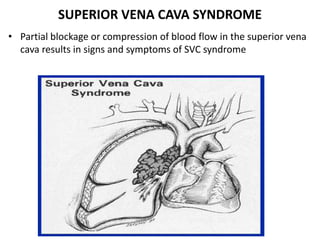
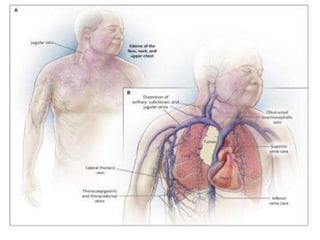
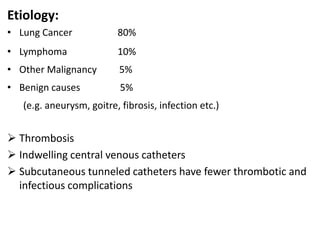
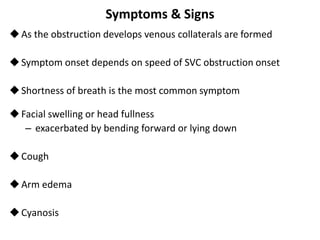
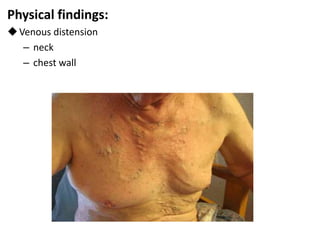
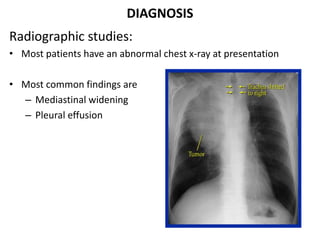
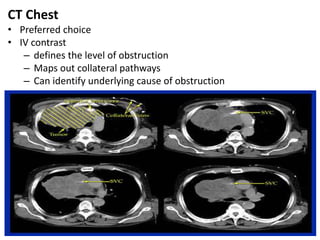
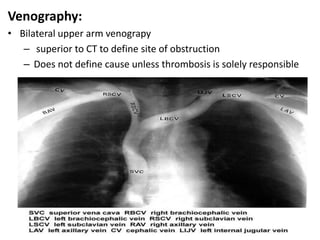
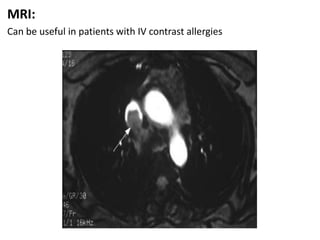
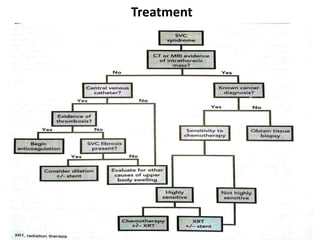
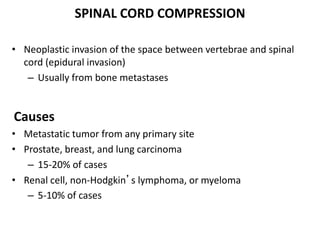
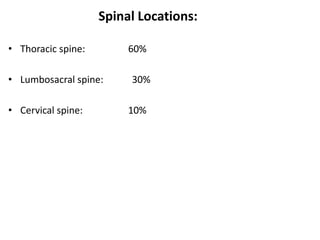
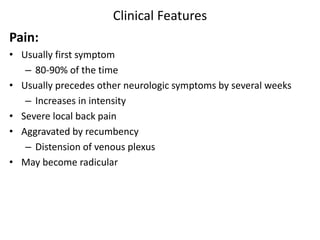
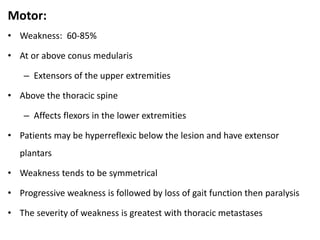
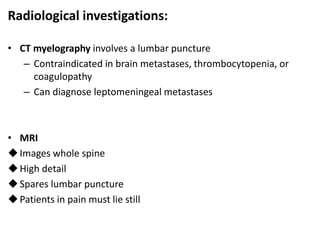
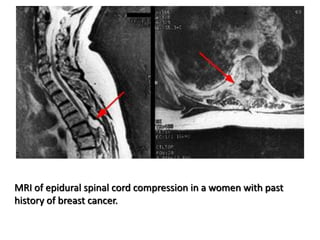
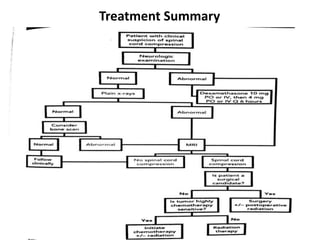
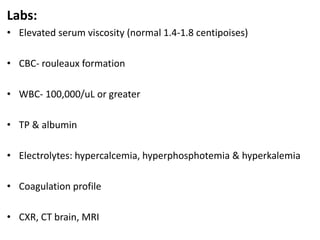
The document discusses several oncological emergencies including tumor lysis syndrome, leucoestasis, hypercalcemia, superior vena cava syndrome, spinal cord compression, and hyperviscosity syndrome. It provides details on the pathogenesis, risk factors, signs and symptoms, diagnostic evaluation and treatment recommendations for each condition. The treatment sections emphasize hydration, uric acid lowering agents, corticosteroids, radiation therapy, surgery, chemotherapy and other supportive measures depending on the specific emergency.