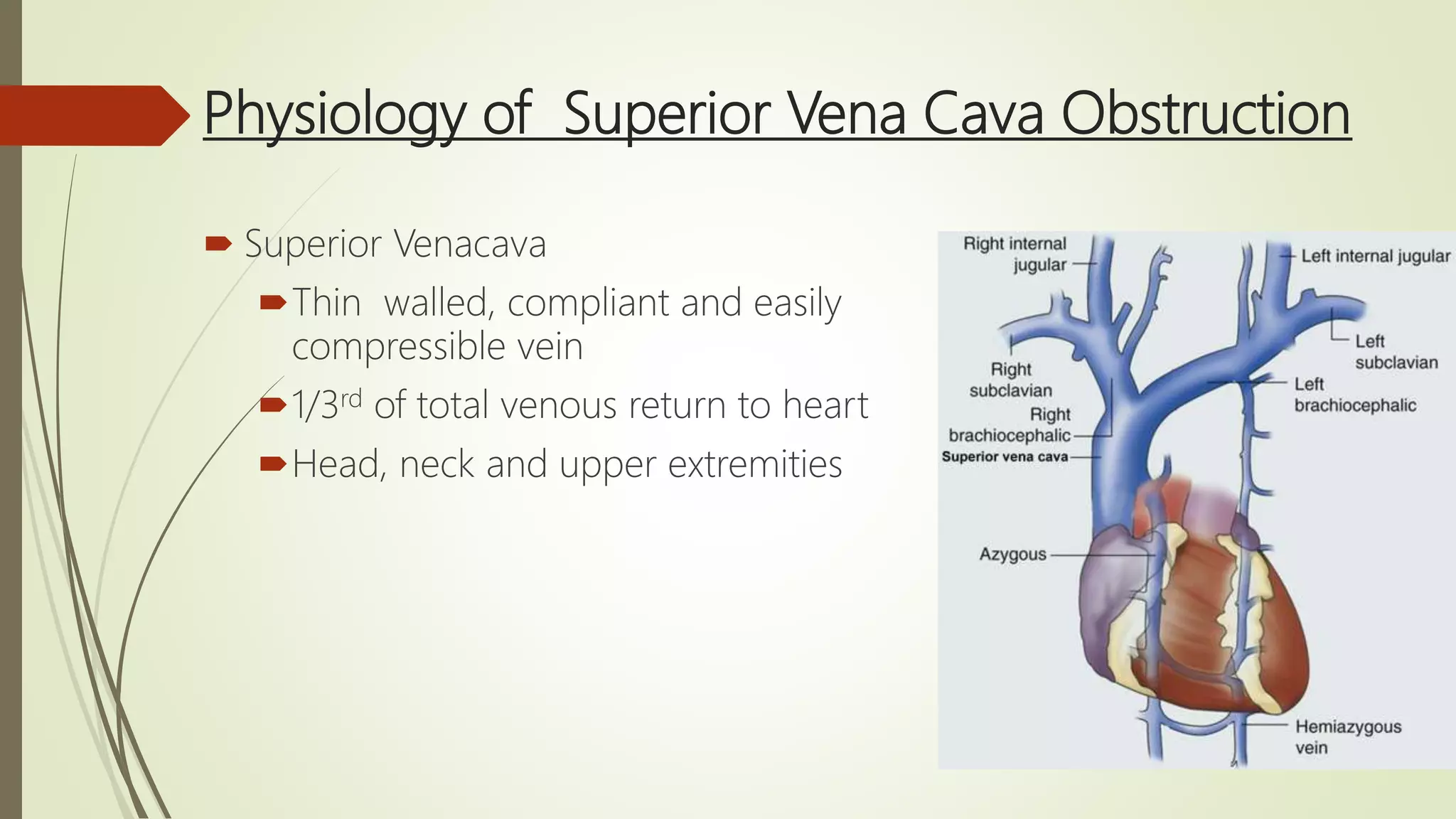
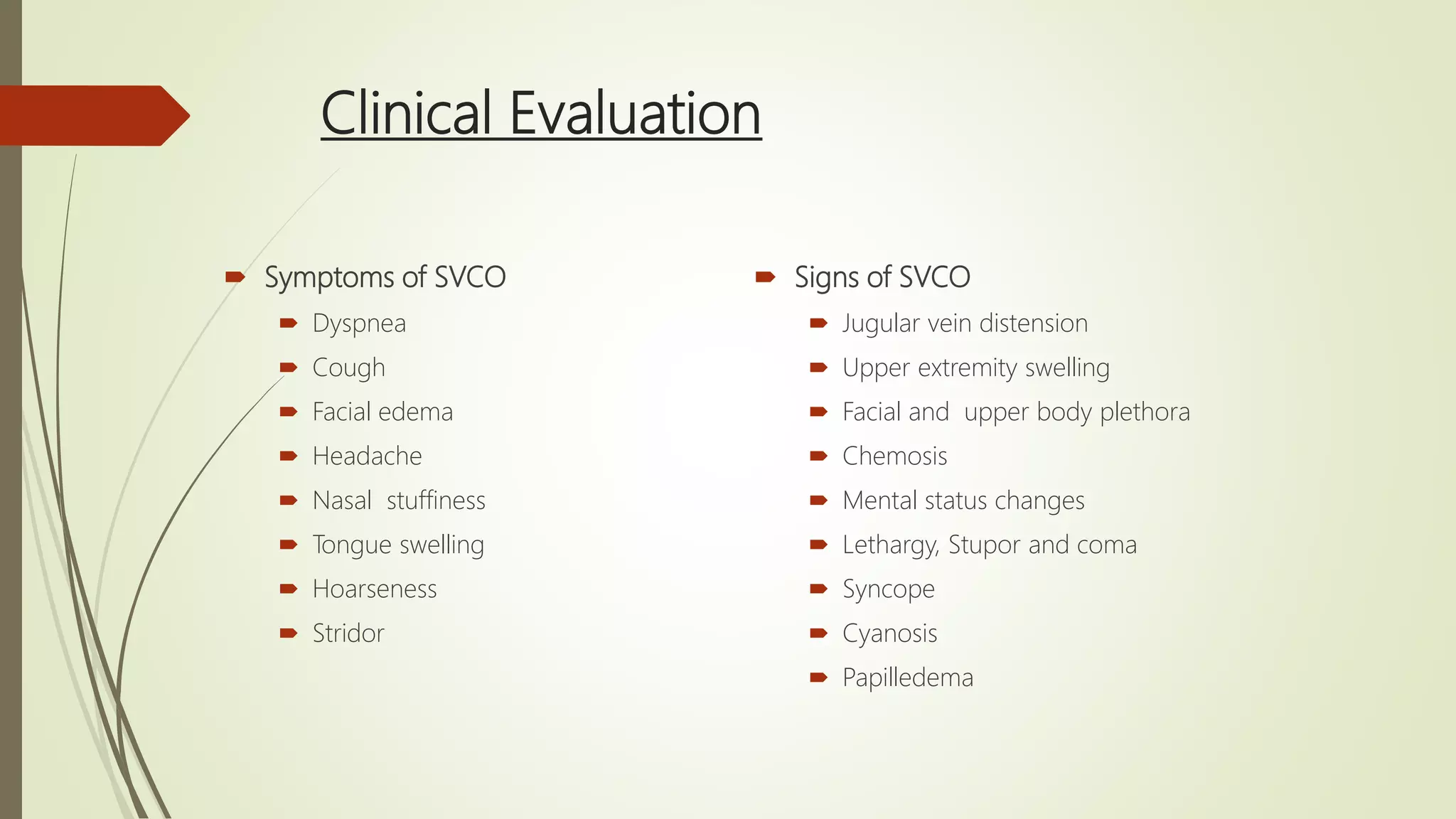
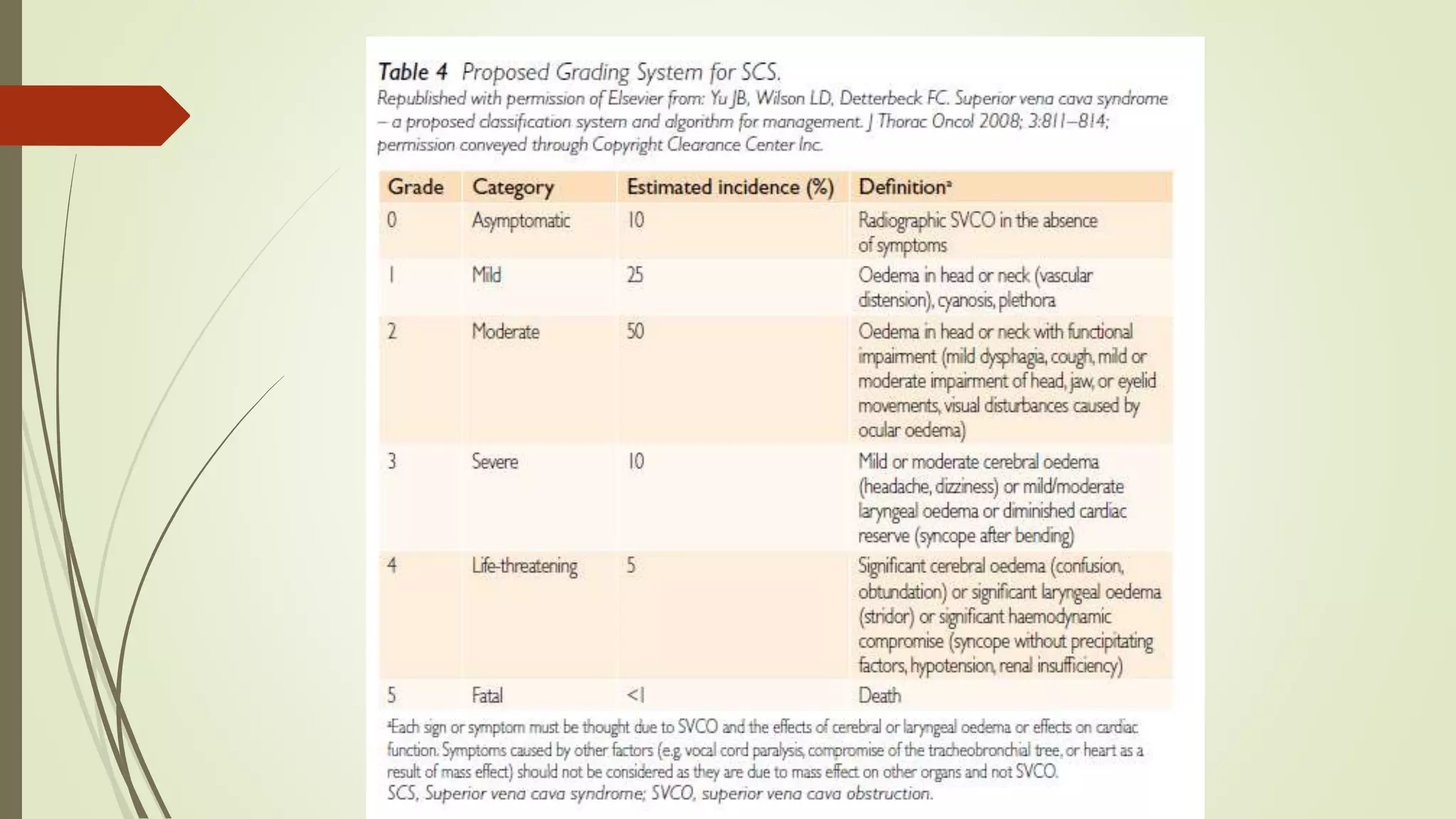
Superior vena cava syndrome (SVCS) is a condition characterized by a range of symptoms due to compression or obstruction of the superior vena cava, predominantly caused by malignancies like lung cancer. Clinical evaluation, imaging, and tissue biopsy guide treatment, which may include stenting, radiotherapy, chemotherapy, or surgery based on underlying pathology. Multidisciplinary management is essential, with emergency interventions required only in life-threatening situations.