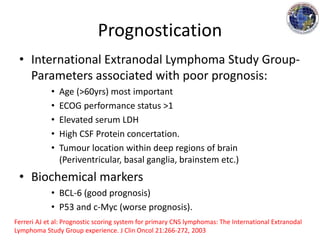
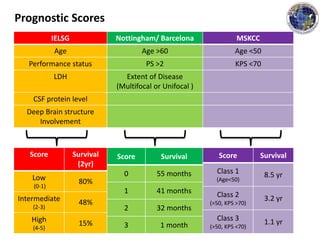
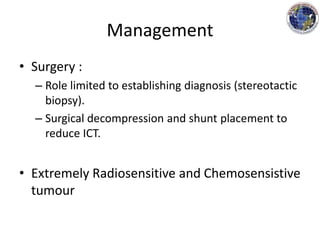
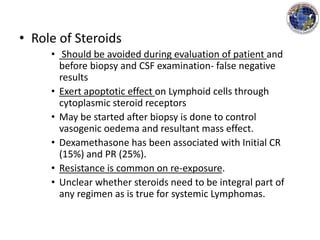
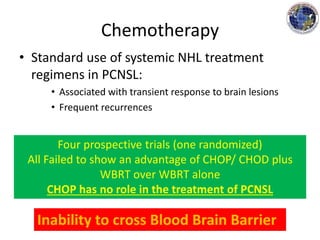
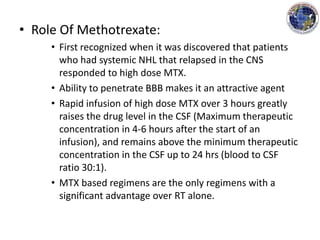
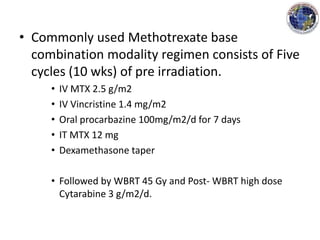
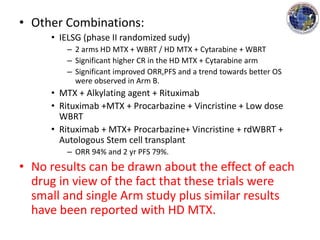
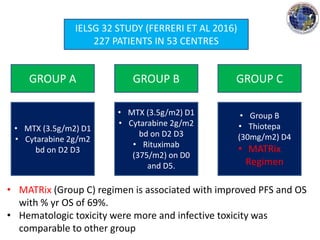
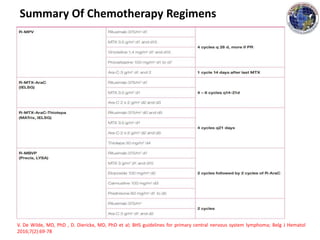
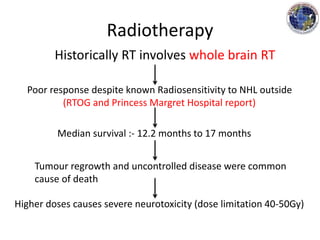
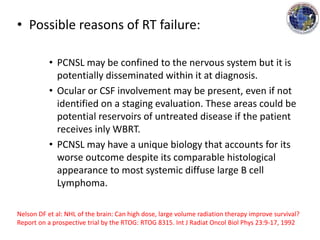
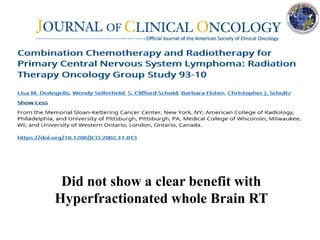
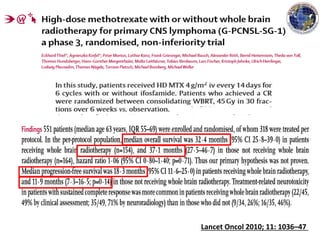
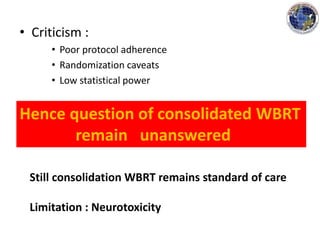
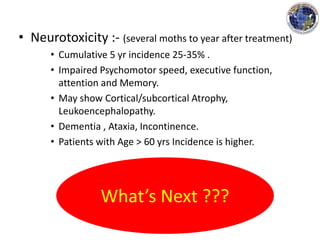
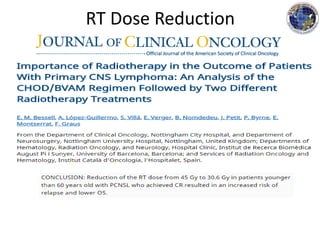
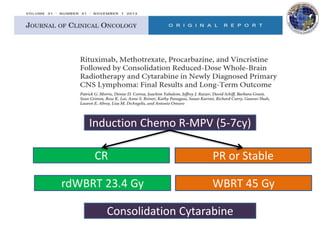
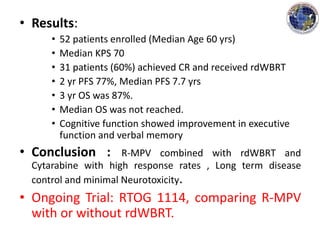
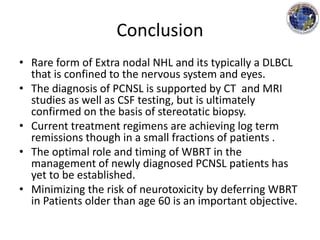
This document discusses the management of primary central nervous system lymphoma (PCNSL). It begins with defining PCNSL and discussing its epidemiology, which includes that it is a rare brain tumor with an increasing incidence in immunocompromised patients. The standard treatment involves high-dose methotrexate-based chemotherapy followed by whole brain radiotherapy, which provides the best outcomes compared to other regimens. Prognostic scoring systems can help determine a patient's prognosis based on factors like age, performance status, lactate dehydrogenase levels, and tumor location. Ongoing research is evaluating adding agents like cytarabine, thiotepa, and rituximab to standard chemotherapy regimens to improve survival further

![• CT scan :- NCCT Iso-Hyperdense on imaging
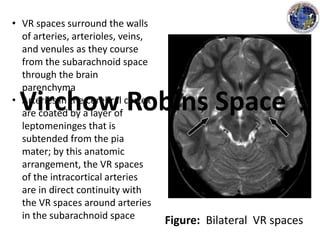
• MRI :-
• Can detect 10% of lesions missed by CT scans.
• T1- iso-hypointense
• T2- (50%shows Hyperintense), in immunocompetent –
Homogenous enhancement.
• Location on imaging (Mostly seen in these areas):
• Hemispheres, Thalamus and Basal Ganglia,Corpus
Callosum, Ventricular region, Cerebellum [ref].
• HIV : Multifocal (d/d CNS infection).
[ref] Kuker W, et al: Primary central nervous system lymphomas (PCNSL): MRI features at
presentation in 100 patients. J Neurooncol 72:169-177, 2005](https://image.slidesharecdn.com/primarycnslymphomappt-180307145149/85/Primary-cns-lymphoma-ppt-12-320.jpg)