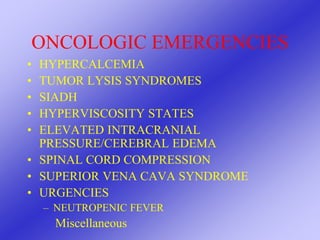
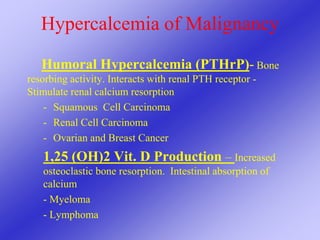
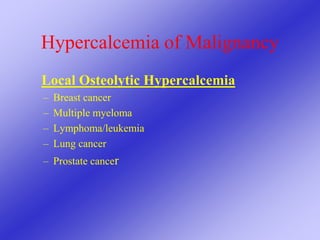
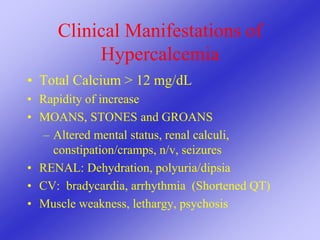
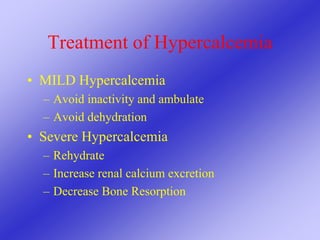
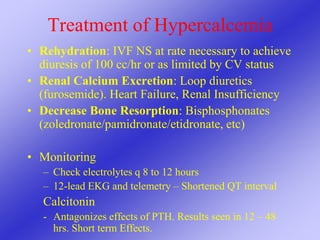
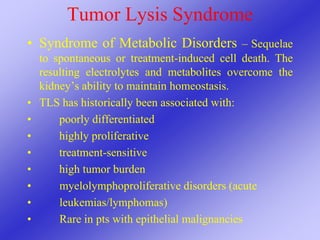
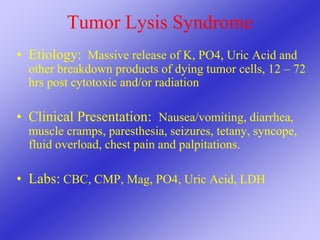
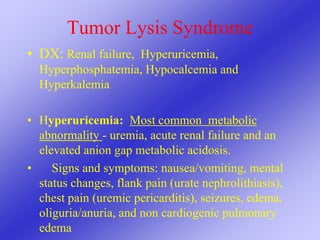
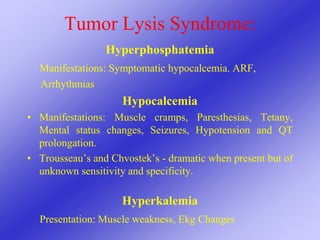
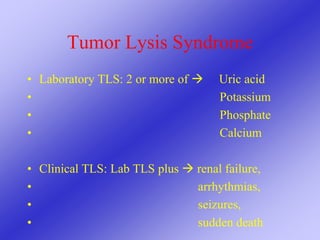
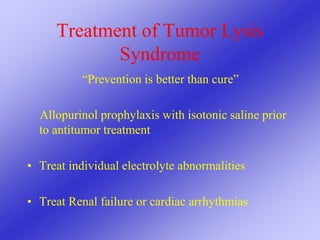
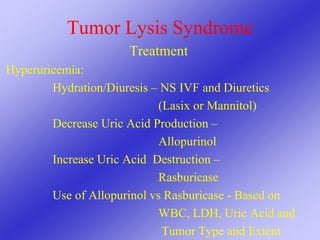
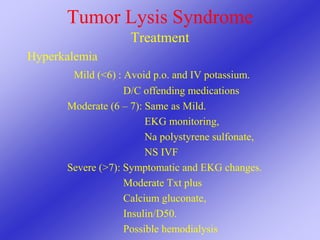
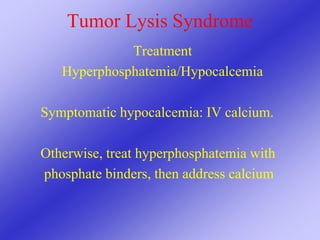
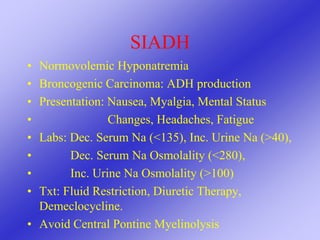
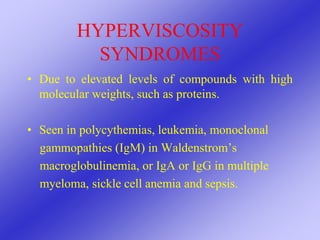
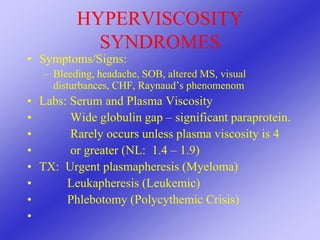
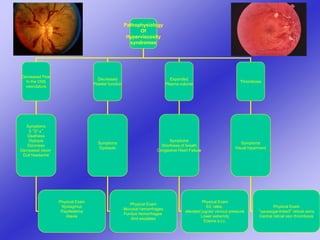
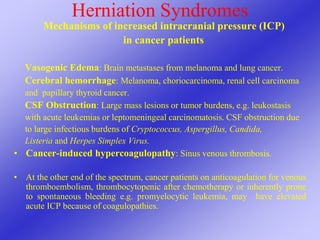
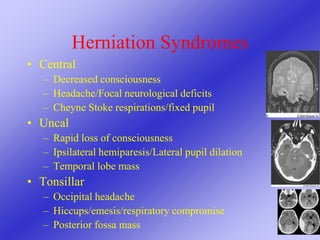
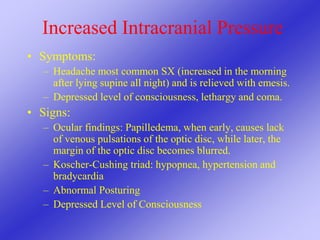
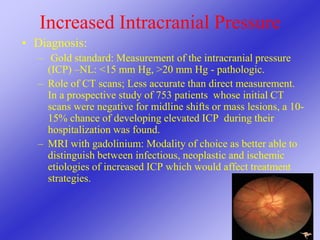
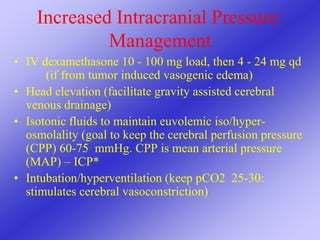
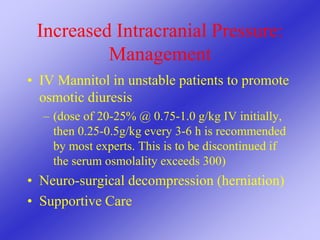
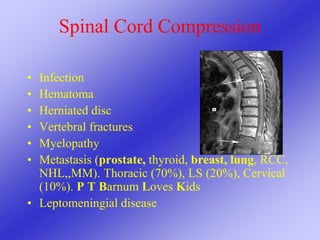
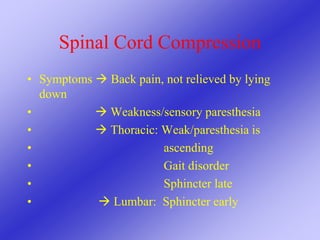
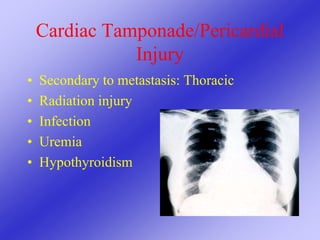
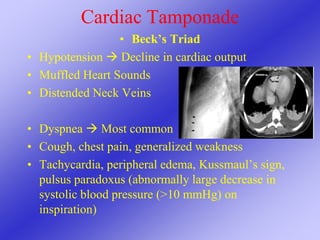
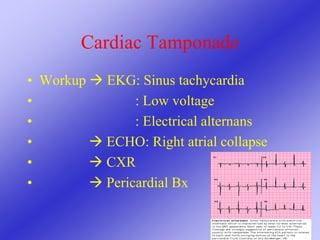
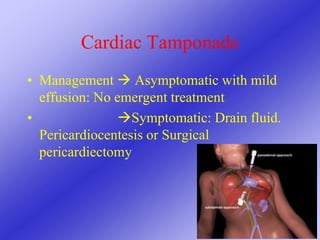
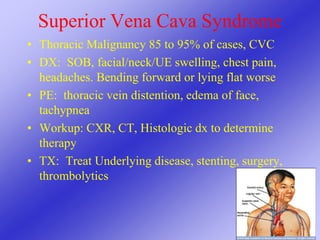
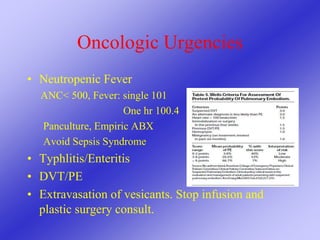
This document provides an overview of various oncologic emergencies including hypercalcemia, tumor lysis syndrome, SIADH, hyperviscosity states, increased intracranial pressure, spinal cord compression, superior vena cava syndrome, neutropenic fever, and other urgencies. For each condition, it discusses causes, clinical manifestations, diagnosis, and treatment approaches. The goal is to educate medical professionals about emergency presentations that may occur in cancer patients and how to appropriately manage these critical situations.