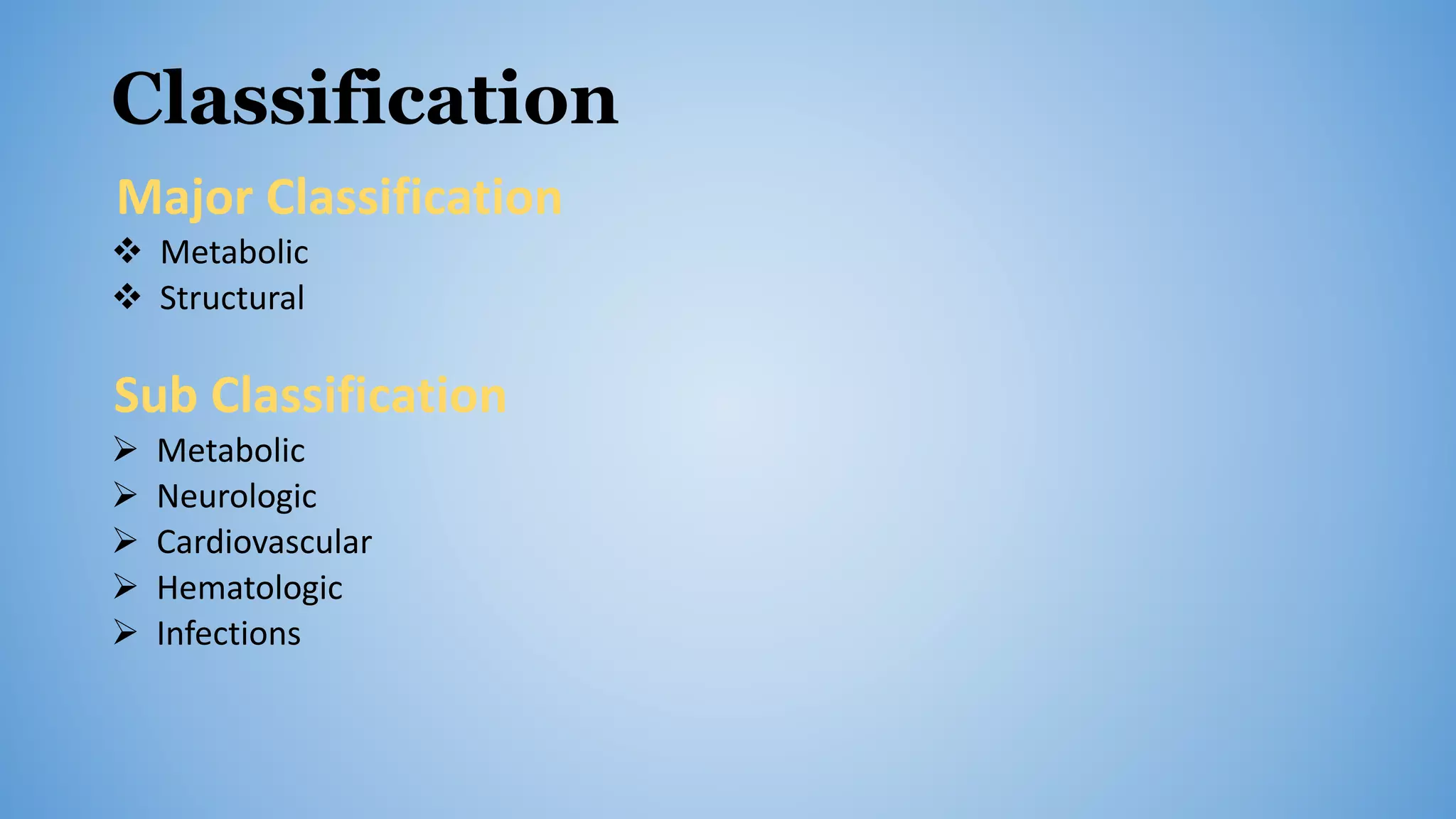
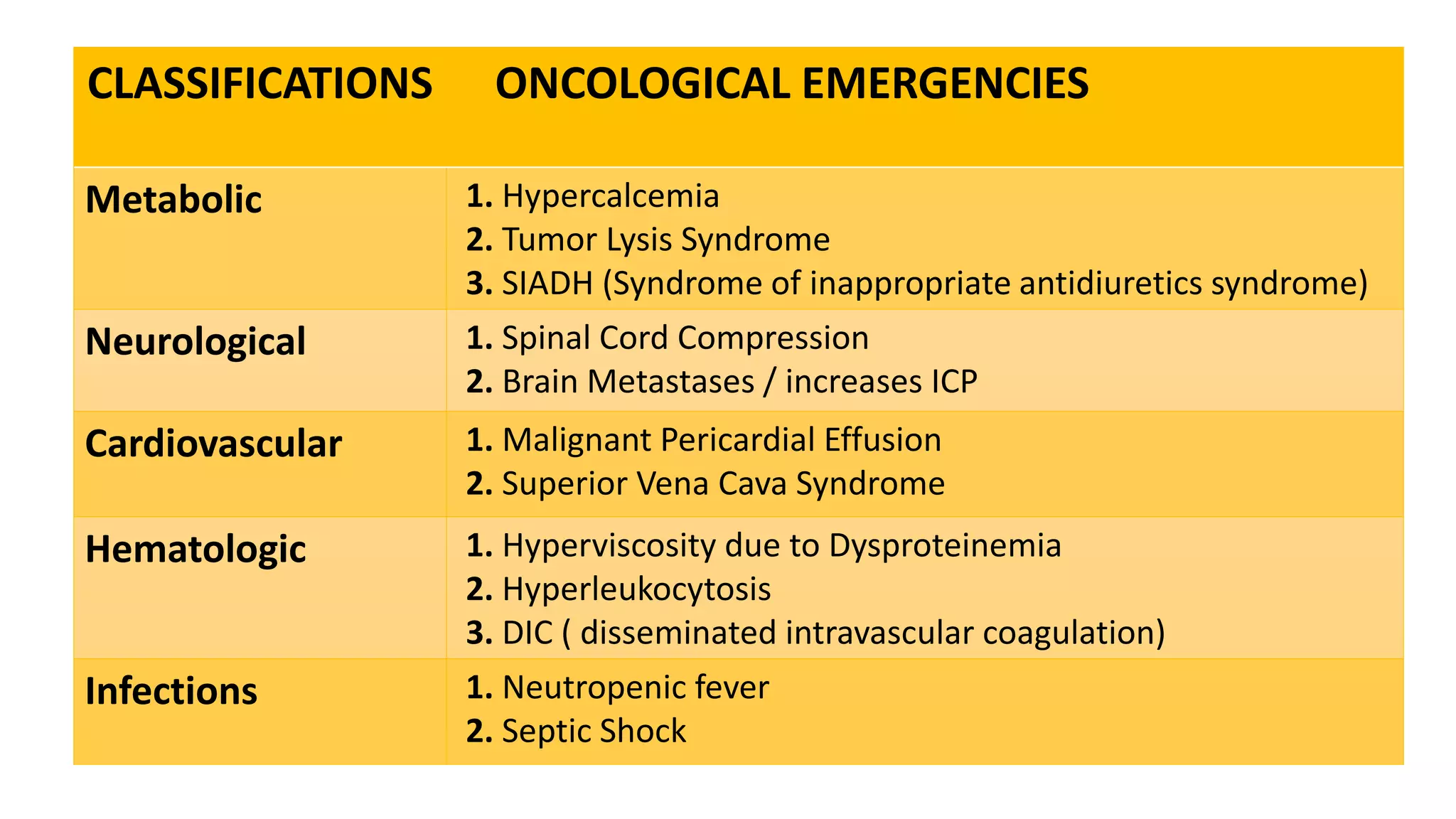
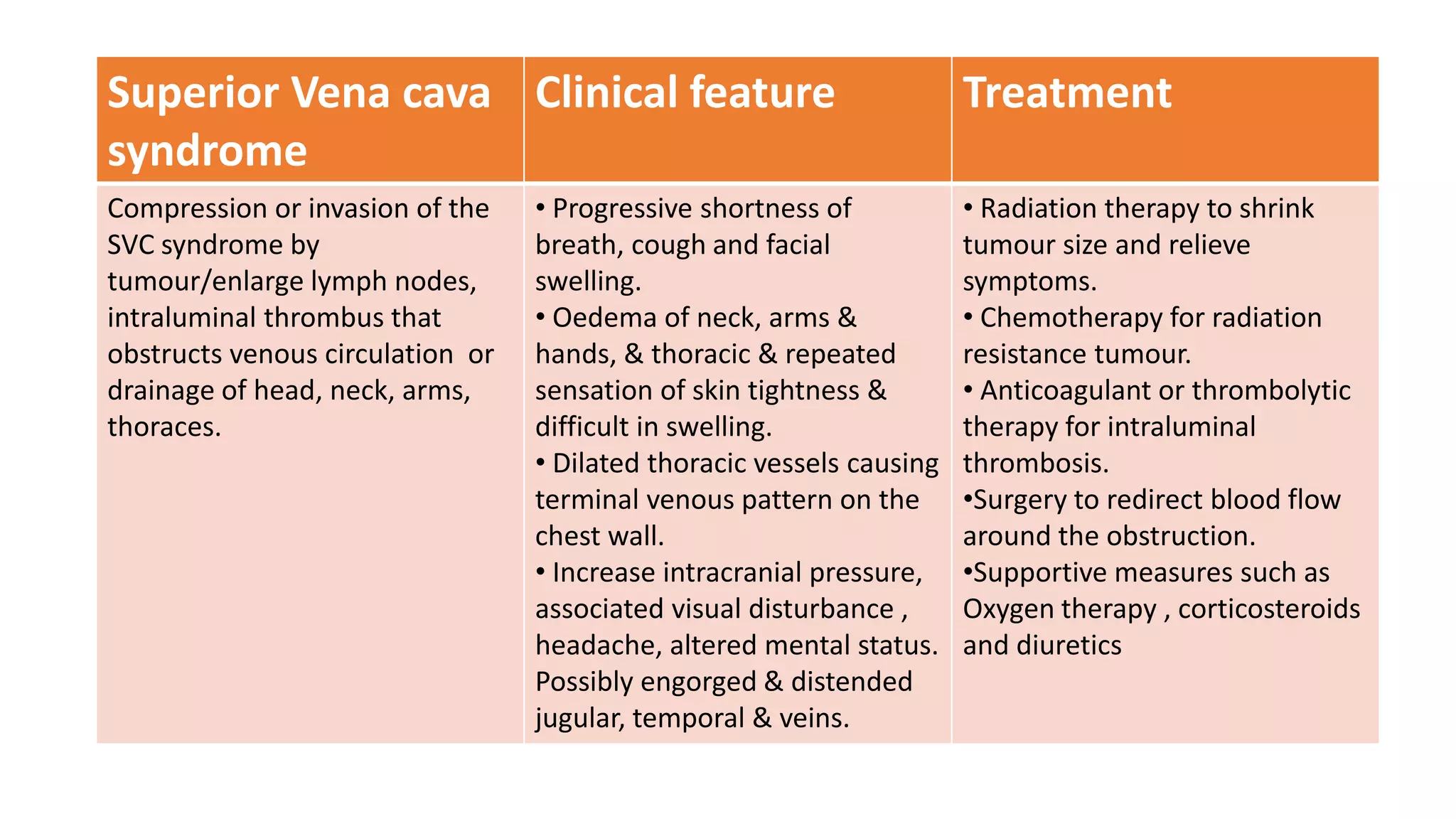
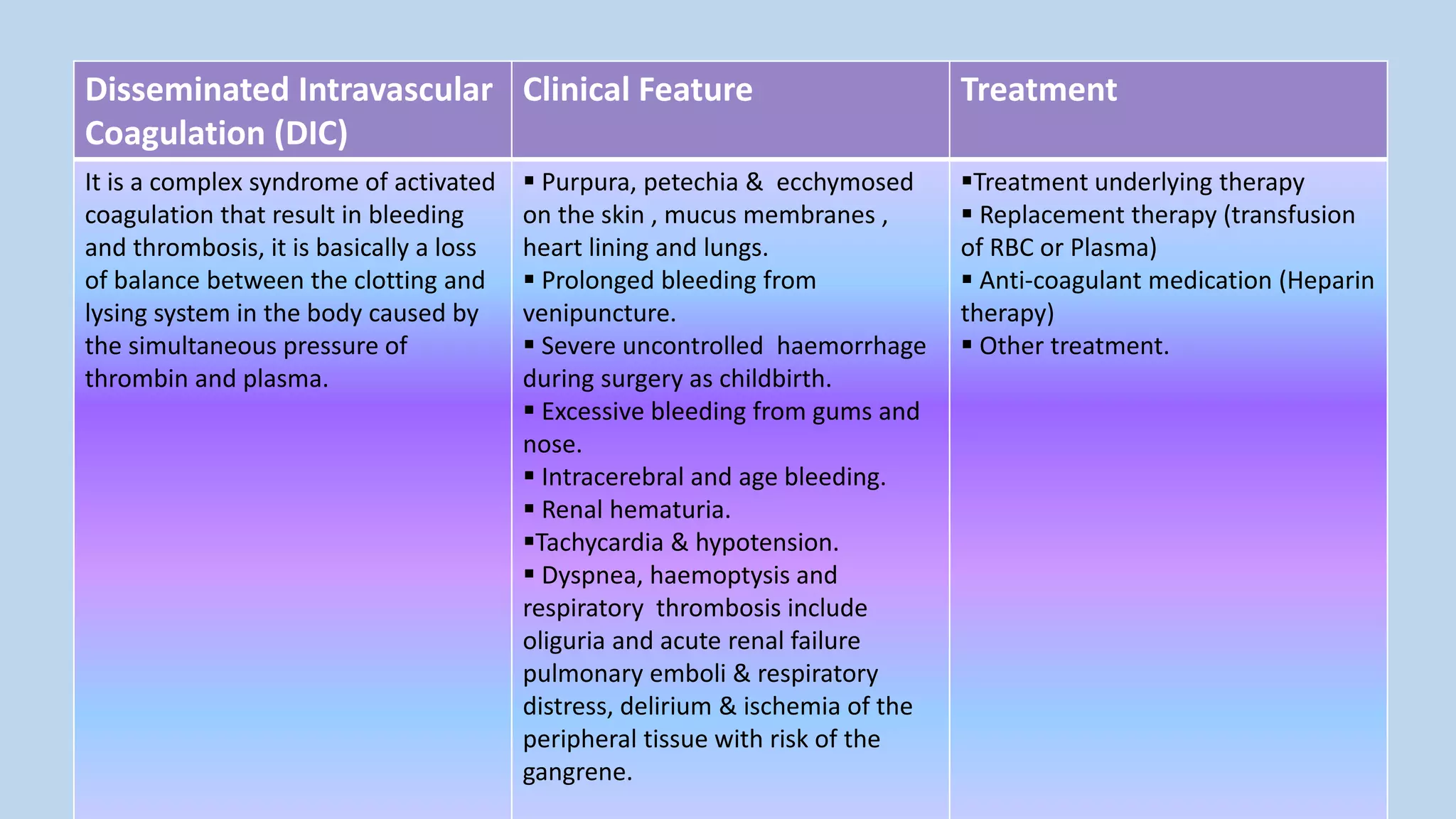
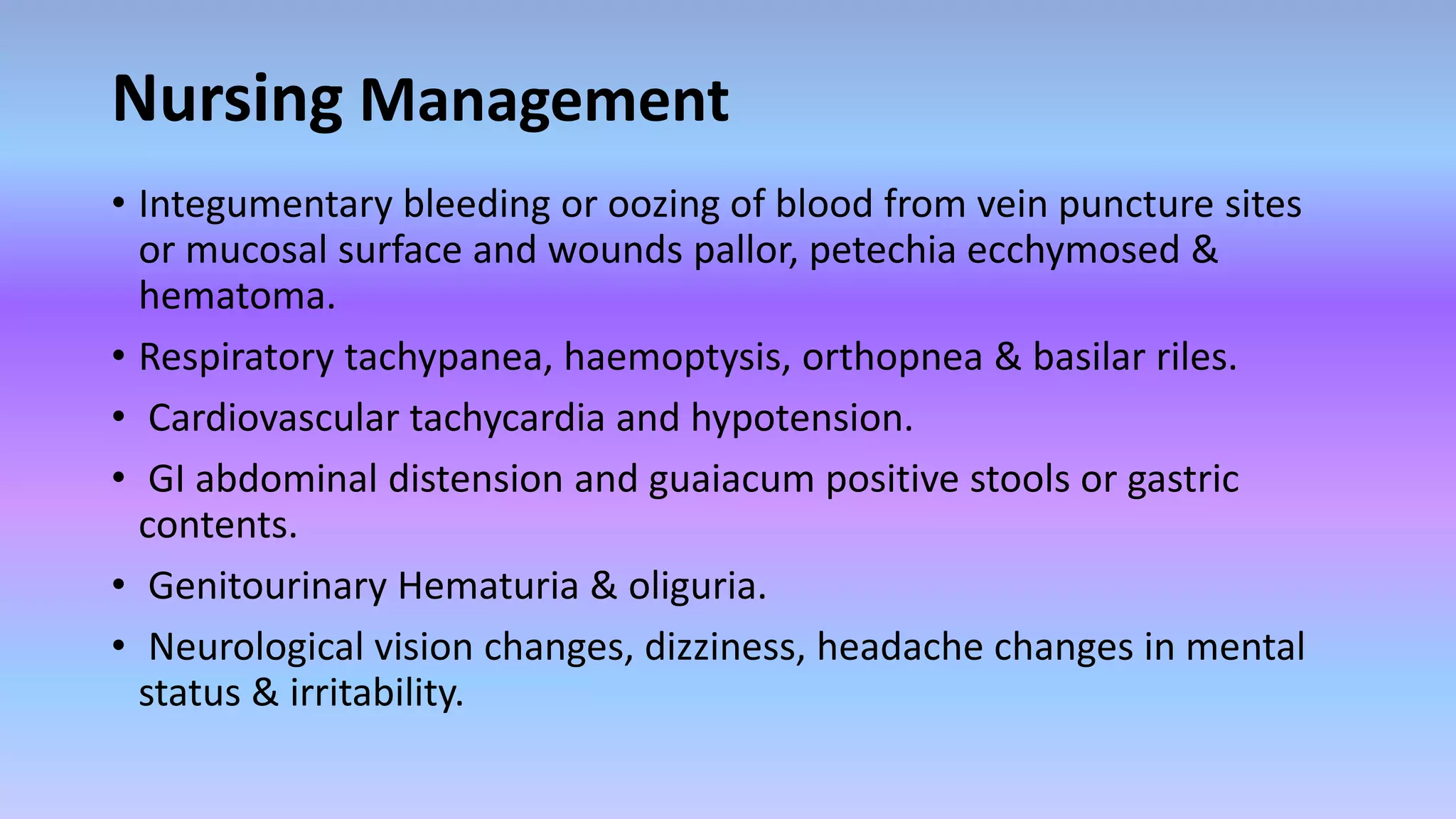
Oncological emergencies can occur in cancer patients from the malignancy or its treatment. They are classified as metabolic, structural, neurological, cardiovascular, hematological or infectious. Some examples include hypercalcemia, tumor lysis syndrome, spinal cord compression, and disseminated intravascular coagulation. Nursing management focuses on monitoring for signs and symptoms, managing complications, educating patients and families, and treating the underlying causes of the emergency.