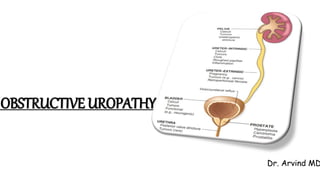
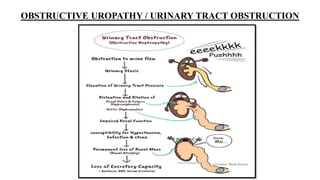
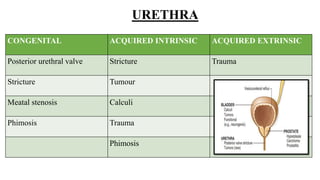
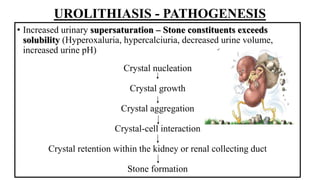
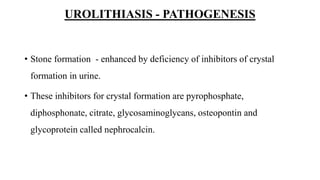
Obstructive uropathy can be caused by various congenital and acquired conditions that obstruct the urinary tract. This obstruction can occur at any level and lead to hydronephrosis or kidney damage if not relieved. Kidney stones, also known as urolithiasis, are a common cause of obstruction and can form from substances like calcium, uric acid, cystine, or struvite bacteria. The formation of stones is due to an imbalance between constituents in urine that cause supersaturation and crystallization. Long-term obstruction can result in hydronephrosis, or dilation of the renal pelvis and calyces, due to continued kidney filtration against resistance. This causes compression of the medullary blood