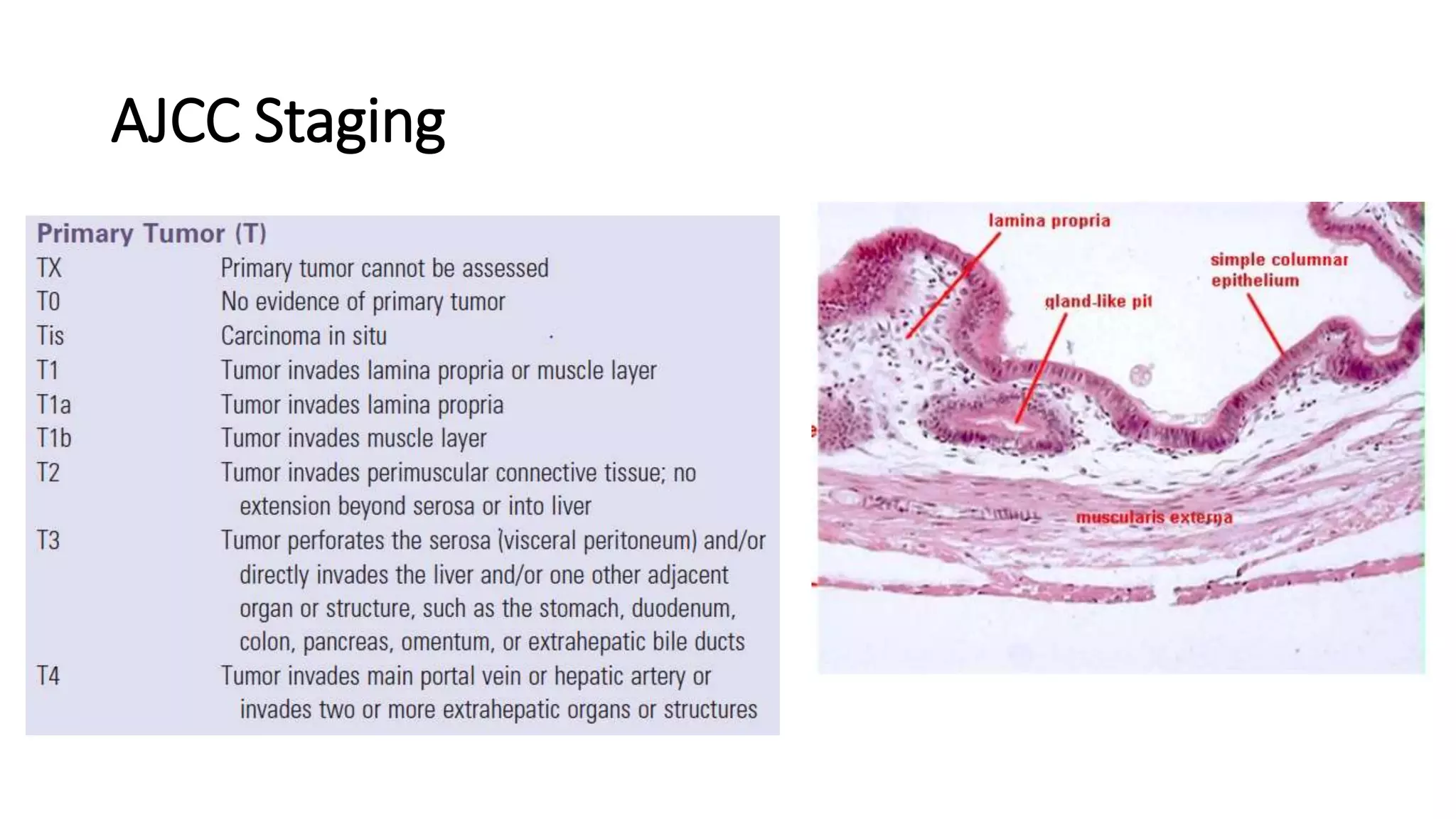
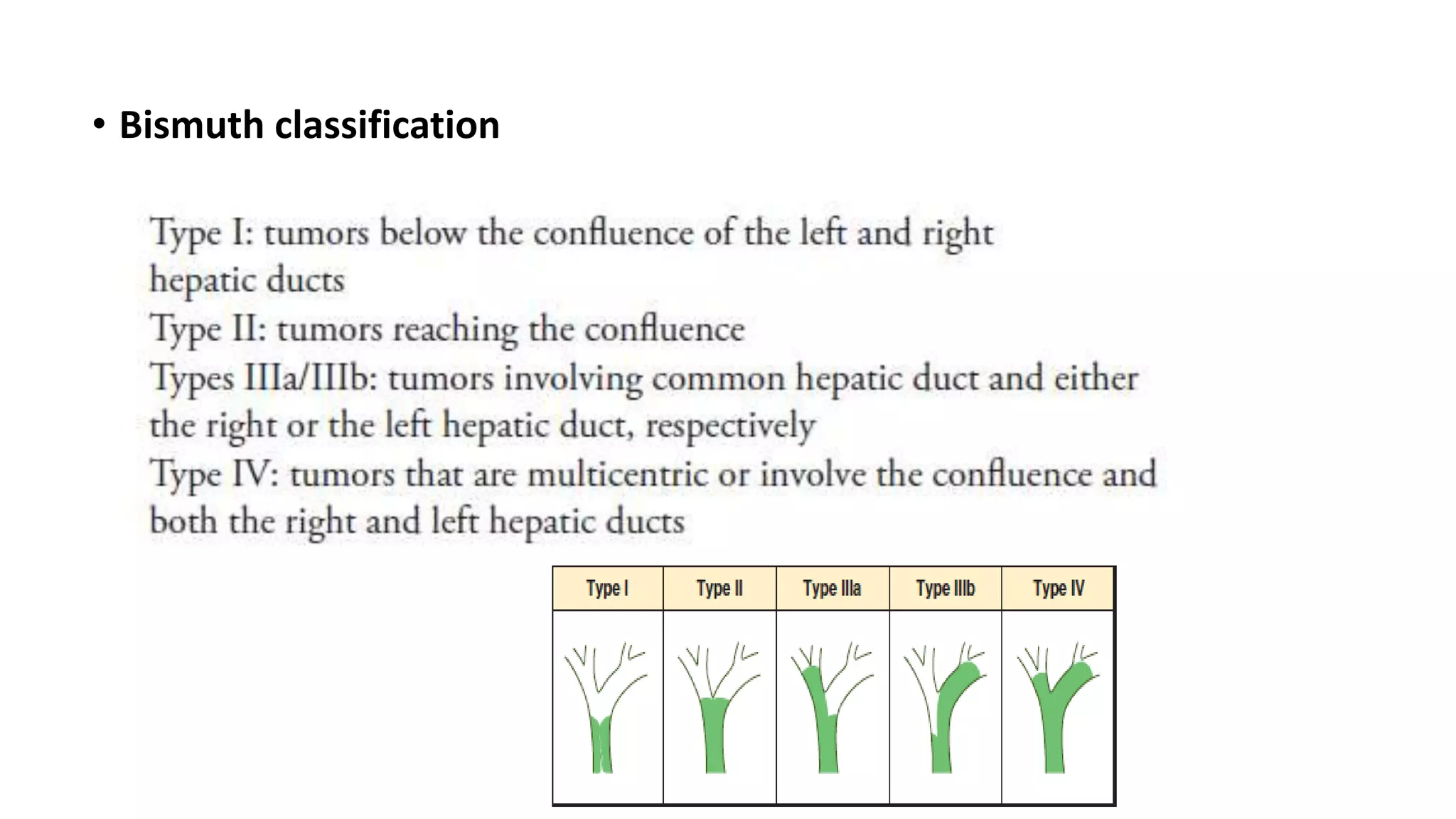
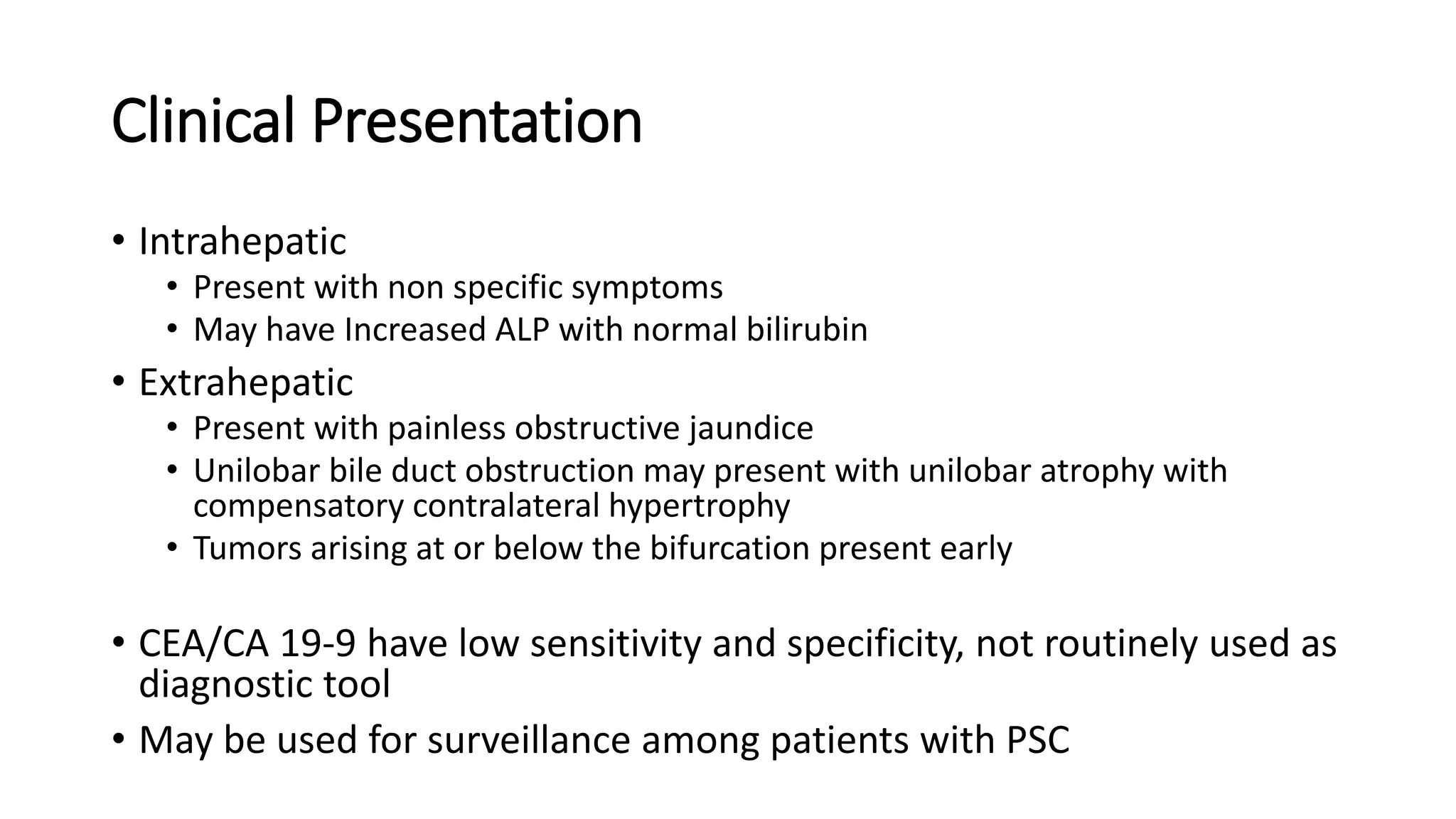
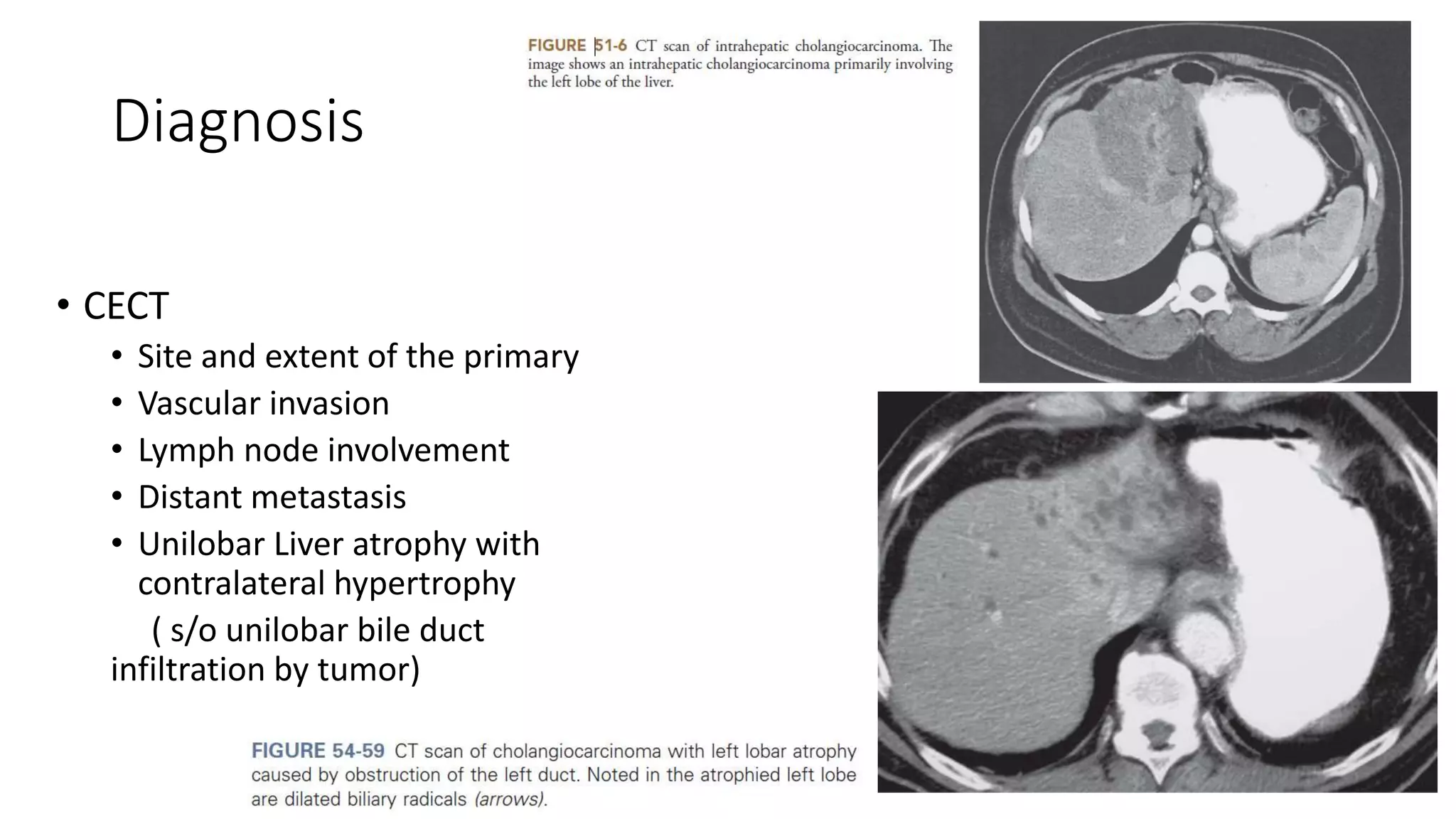
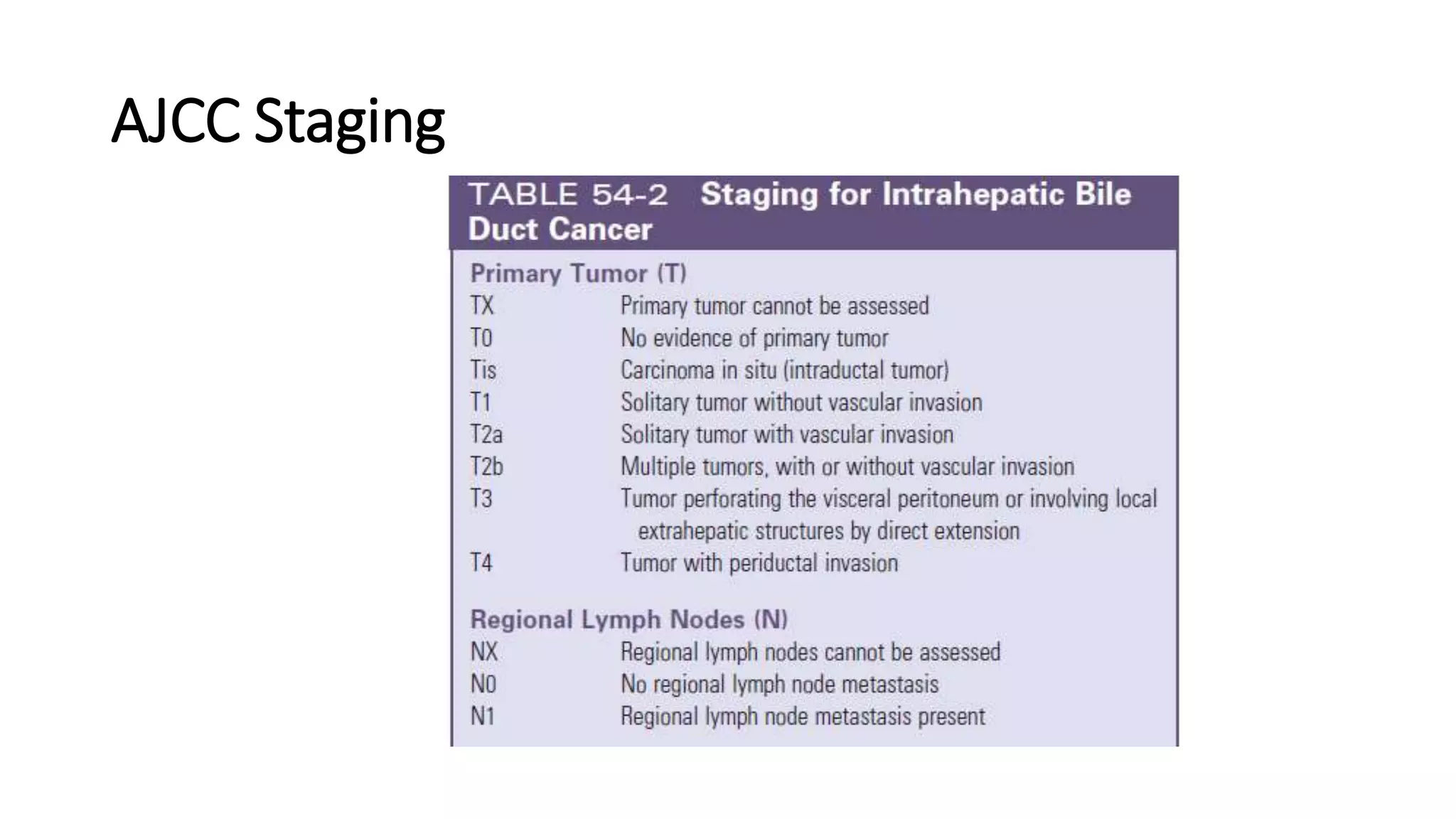
The document discusses biliary tract cancer, highlighting its higher prevalence in North India and noting that gallstones are a significant risk factor, though most patients with gallstones do not develop cancer. It outlines the staging and surgical management protocols for different types of biliary tract cancers, emphasizing that complete surgical resection is the only curative treatment. Additionally, the document touches upon clinical presentation, diagnosis, and various treatment options including palliation and adjuvant therapy.