Irrigation!
Surgeon: Thank you!
9
10
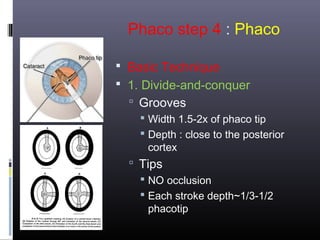
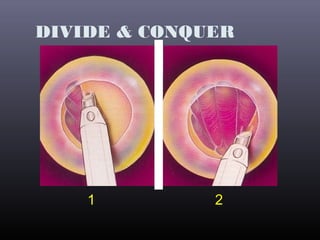
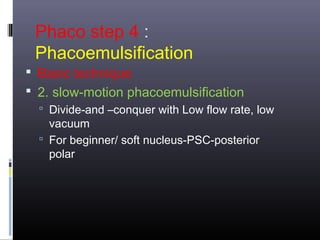
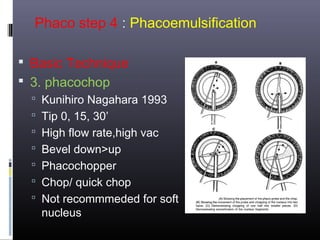
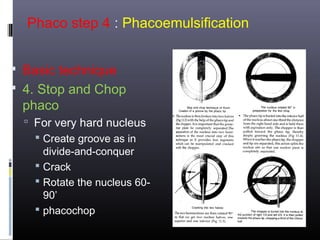
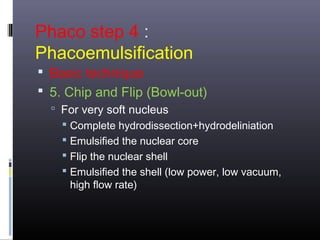
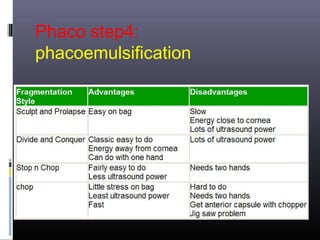
�Phaco step 4 : Phaco
Basic Technique
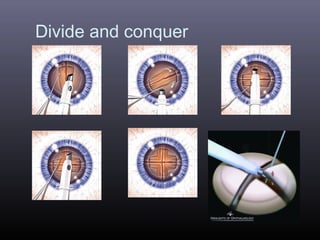
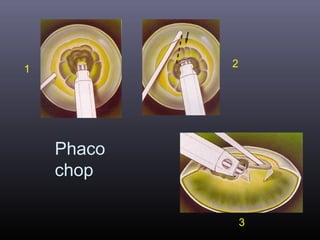
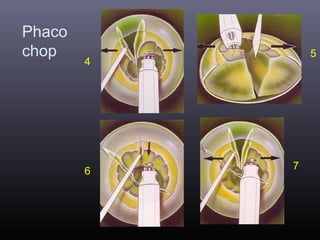
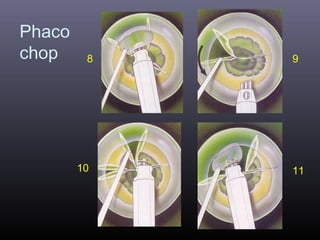
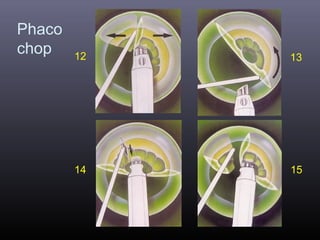
2. Phaco chopping
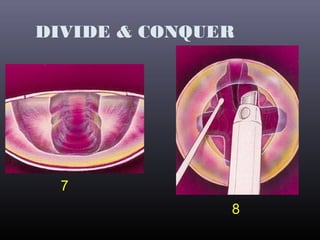
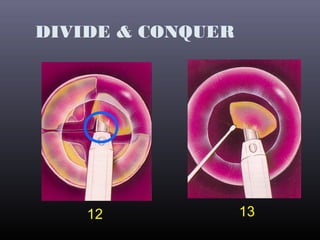
Chopping the nucleus into small pieces
Tips
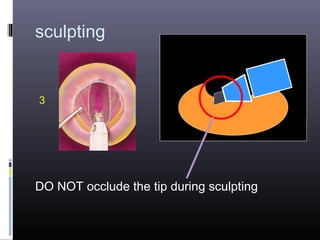
NO occlusion
Each stroke depth~1/3-1/2 phacotip
Chop into small pieces
Irrigate frequently
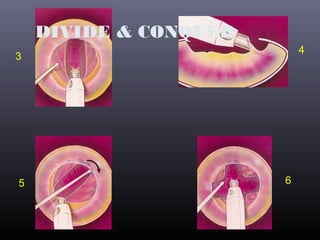
�Phaco chopping
1
2
3
4
5
6
7
8
9
10
11
12
13
14