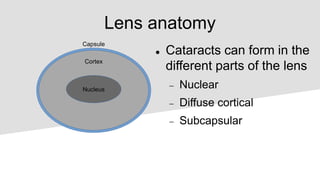
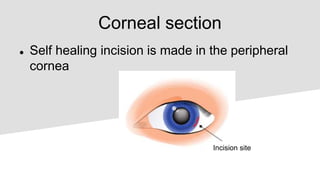
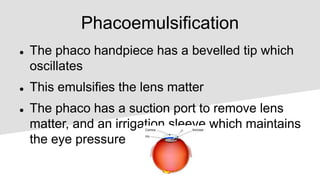
This document provides an overview of cataracts, including definition, types, risk factors, pathophysiology, presentation, management, and complications. A cataract is a clouding of the lens in the eye that impairs vision. The most common type is age-related cataract. Surgery involves removing the cloudy lens and replacing it with an intraocular lens. Potential complications include failure of the corneal incision to seal and tears in the lens capsule that allow vitreous to enter the anterior chamber.