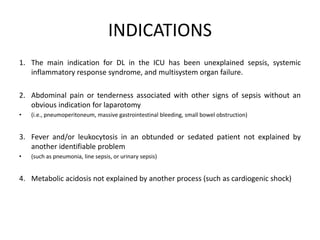
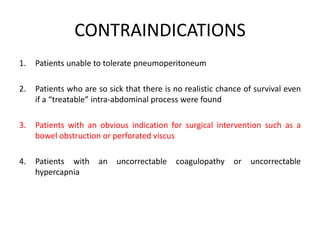
Diagnostic laparoscopy can be used safely in the ICU to diagnose intra-abdominal pathology in critically ill patients without moving them to the operating room. It has a high diagnostic accuracy of 90-100% and can help avoid unnecessary laparotomies in 36-95% of cases. While it has some limitations for retroperitoneal processes, diagnostic laparoscopy is recommended for use in the ICU when an intra-abdominal catastrophe is suspected but cannot be ruled out noninvasively, or to evaluate for conditions like acalculous cholecystitis or ischemic bowel. Any complications are typically minor and it does not increase mortality, which remains high for the critically ill ICU patient population.