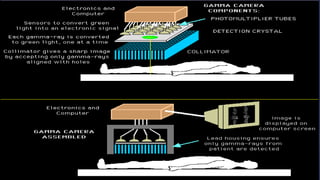
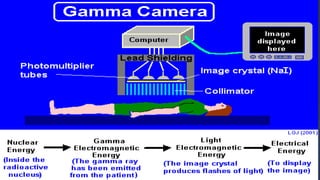
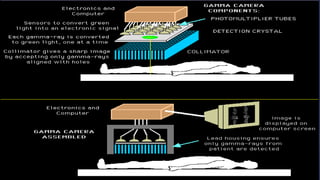
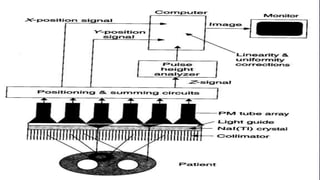
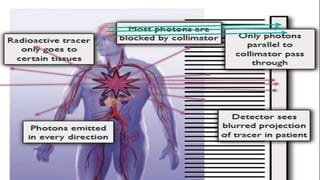
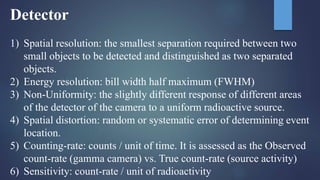
Nuclear medicine is a medical specialty that utilizes radiation from radioactive tracers for diagnostic and therapeutic purposes, often employing radiopharmaceuticals that quickly lose radioactivity and are safely eliminated from the body. Gamma cameras are key imaging devices in this field, capturing both static and dynamic images of tissues using gamma rays emitted from these tracers. The document also discusses the principles of radiation types, half-lives, detection technologies, and considerations for minimizing patient exposure to radiation during imaging procedures.