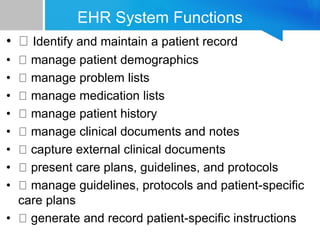
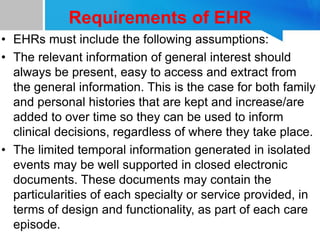
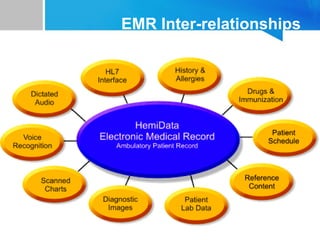
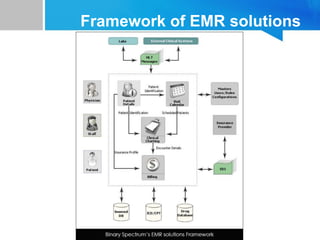
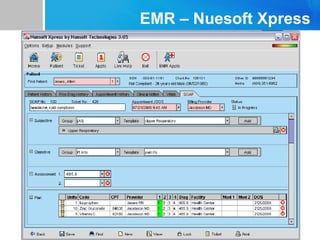
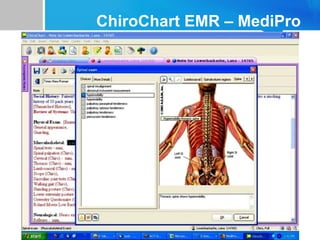
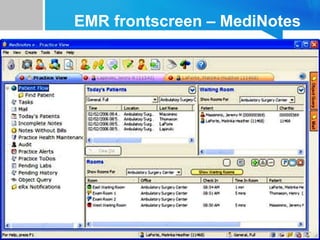
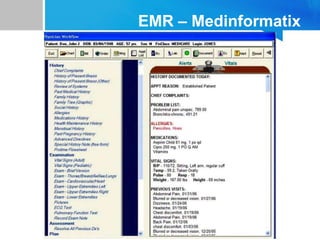
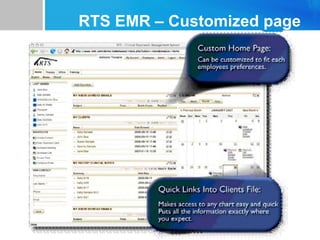
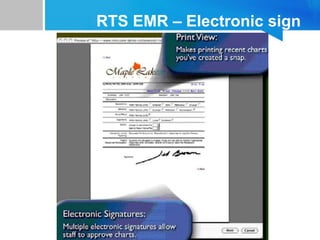
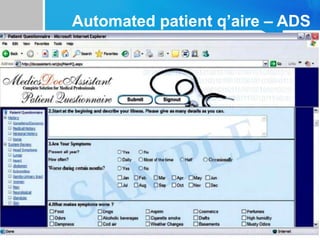
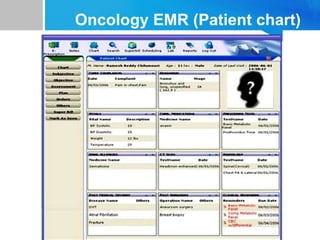
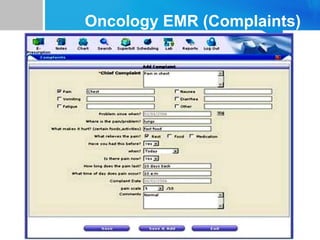
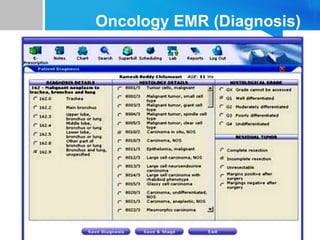
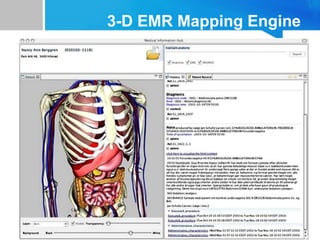
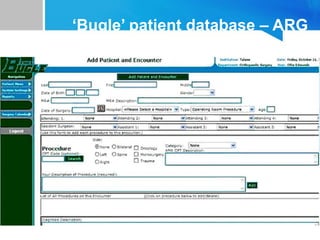
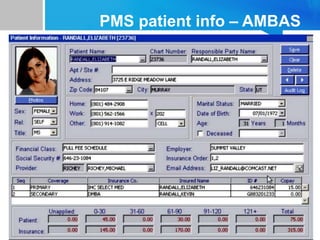
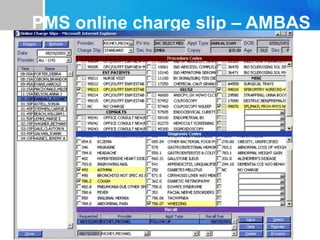
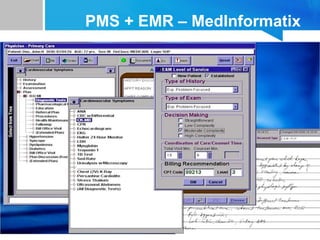
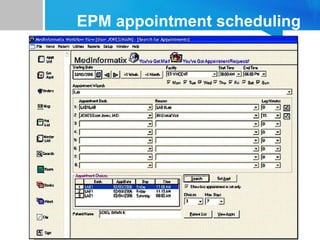
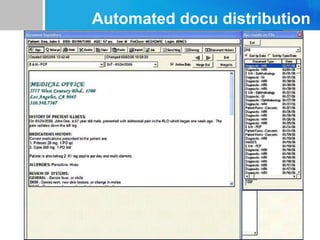
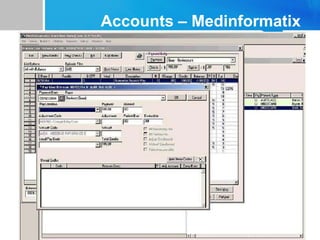
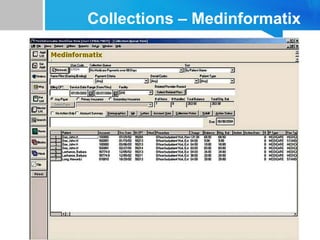
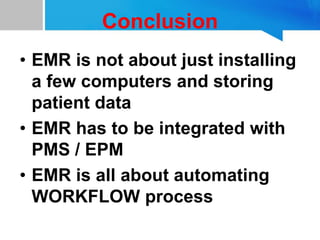
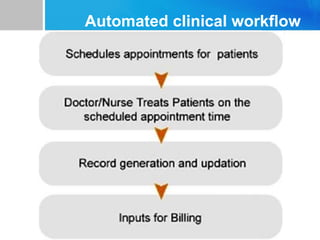
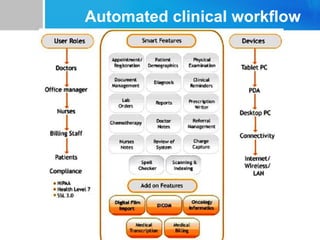
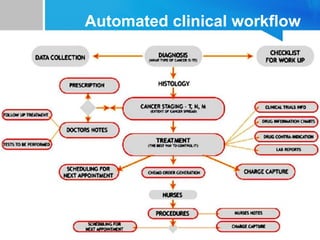
The document discusses electronic medical records (EMRs), defining them as digital versions of patients' paper medical charts that contain their medical history, diagnoses, treatments, test results, and other clinical data. EMRs allow authorized medical providers to securely access a patient's comprehensive medical record electronically. The document also outlines the key components, functions, and benefits of EMR systems, such as automating workflows, integrating with other healthcare IT systems, and facilitating data sharing across providers to support comprehensive patient care.