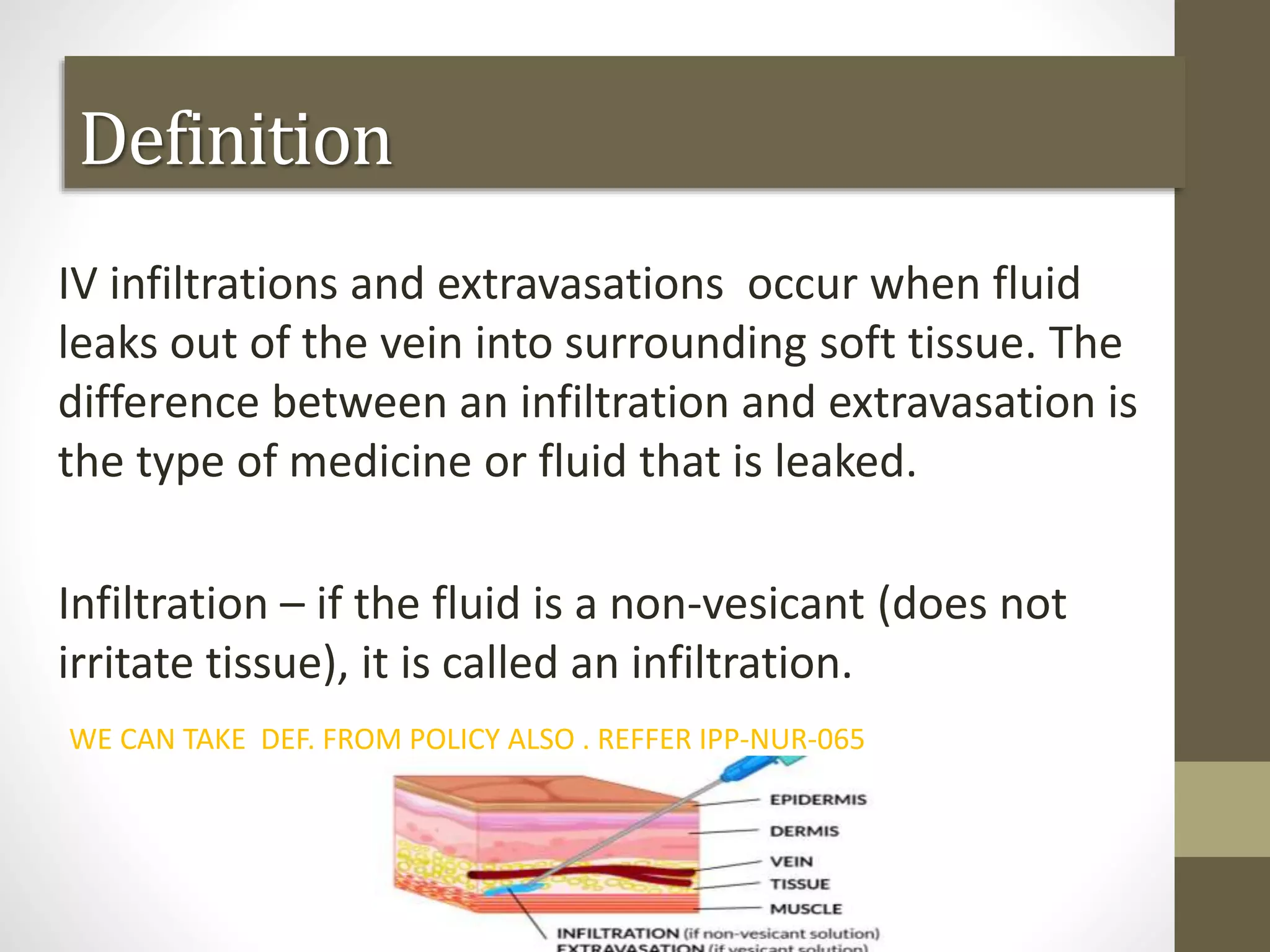
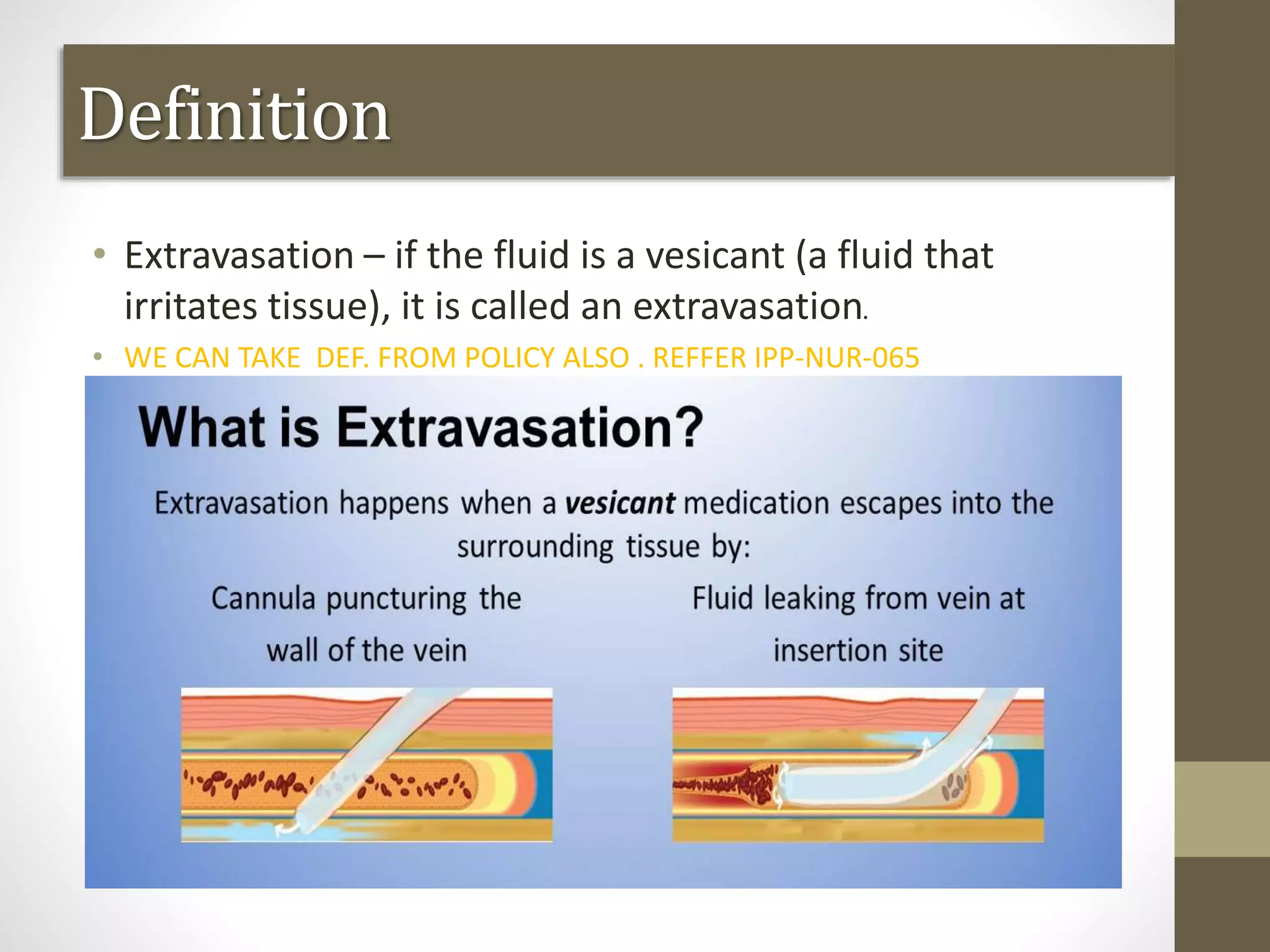
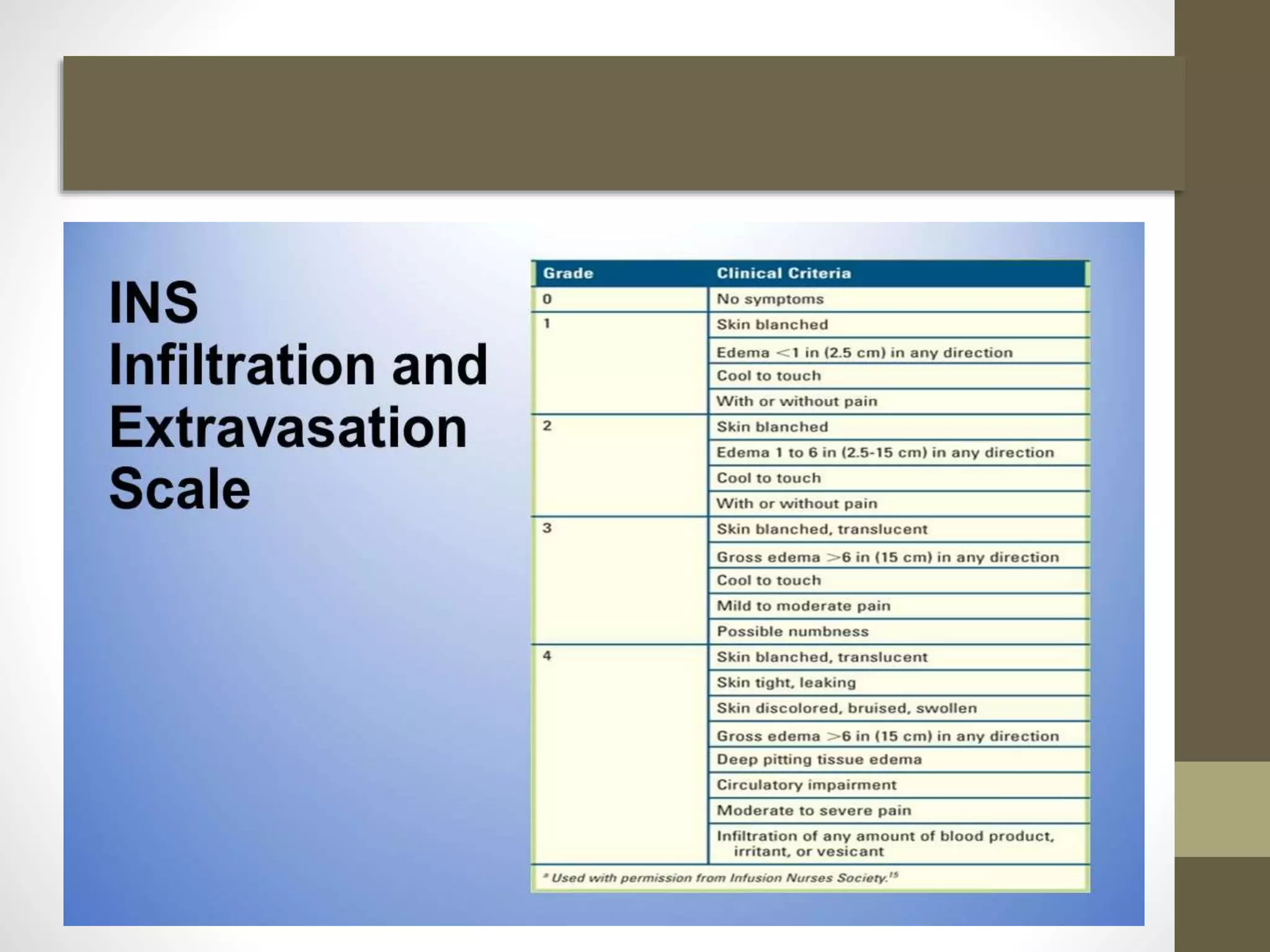
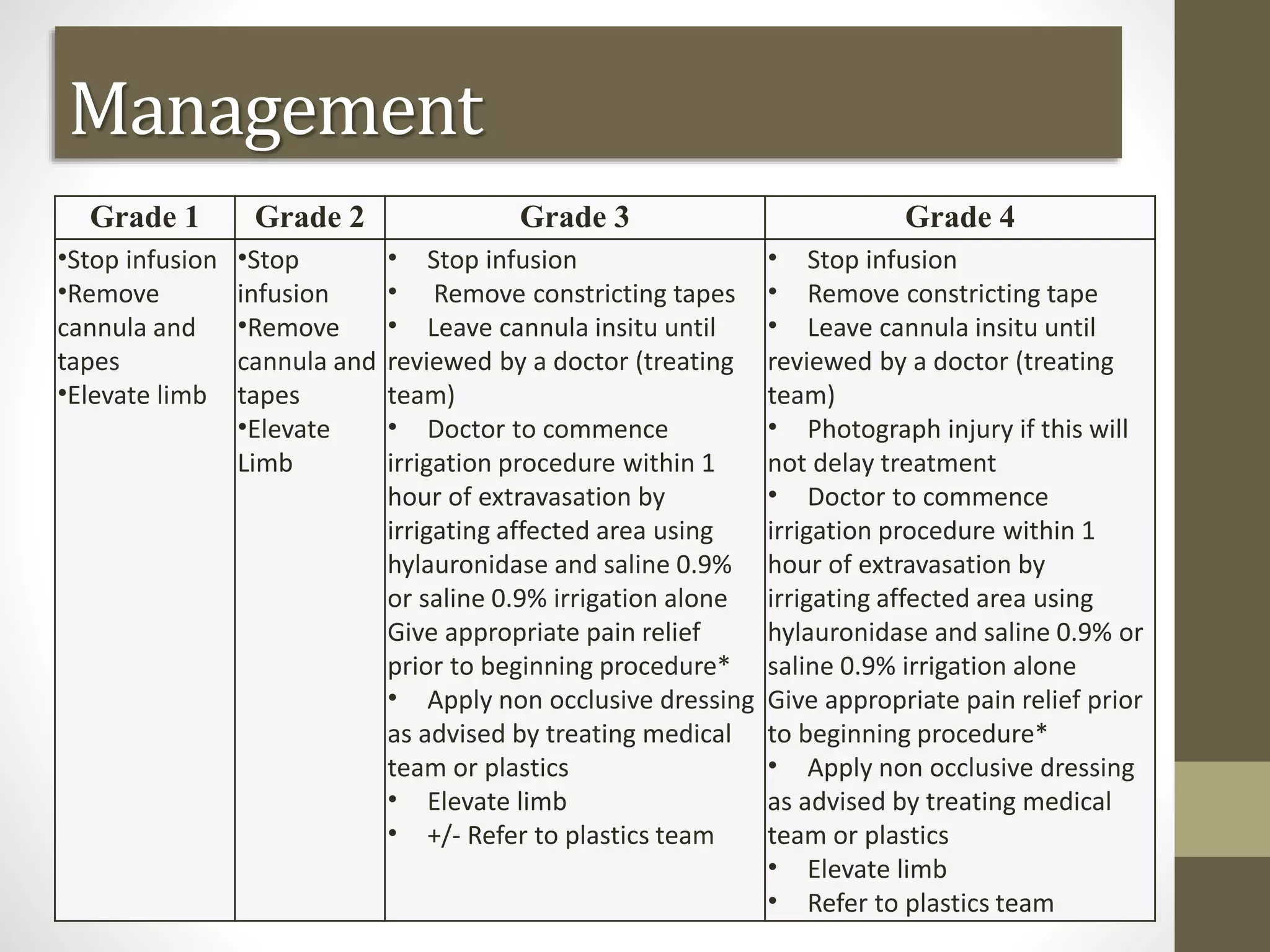
This document discusses IV infiltration and extravasation. It defines these terms and describes signs and symptoms. It outlines categories of infiltration and extravasation and explains prevention, management, and treatment. Precautions are discussed for peripheral and central lines. High risk patients and detection methods are covered. General treatment includes stopping the infusion, aspirating residual drug, elevating the limb, and applying compresses. Management of specific non-chemo drug extravasations is also reviewed. The conclusion emphasizes the importance of prevention and successful treatment to avoid injury.