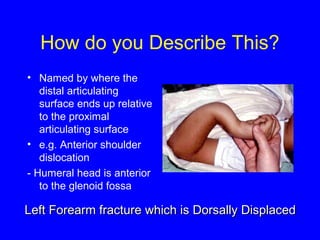
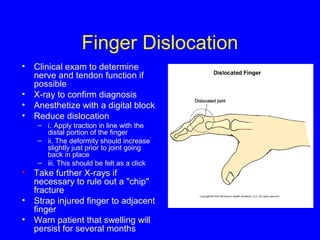
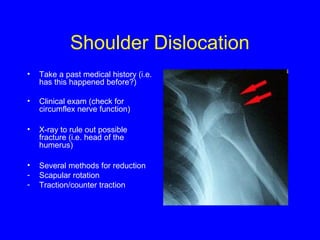
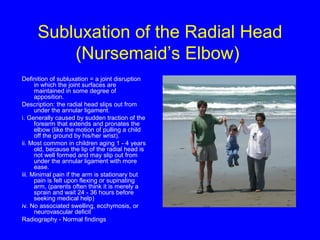
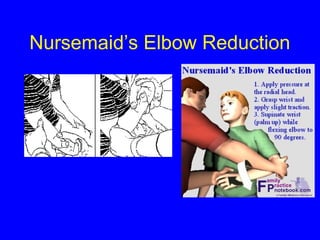
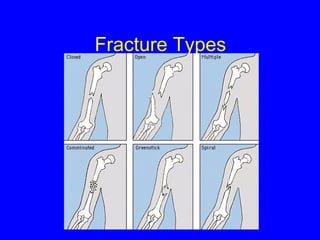
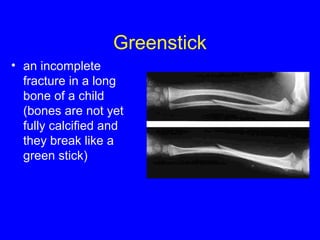
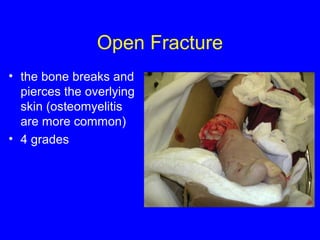
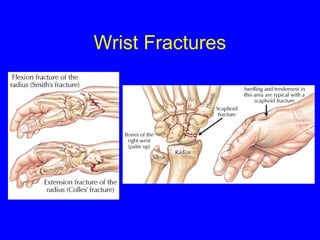
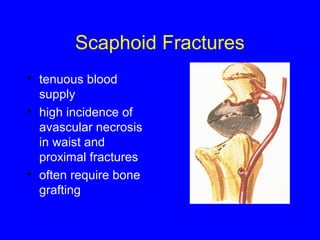
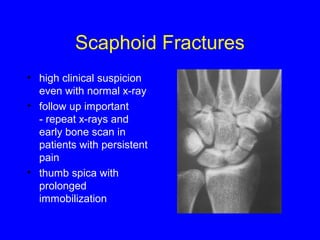
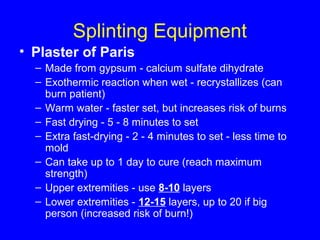
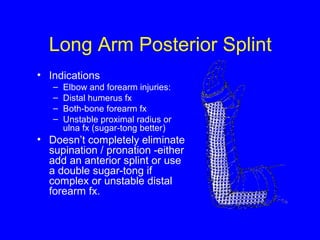
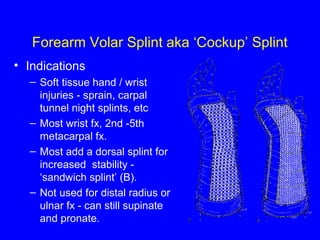
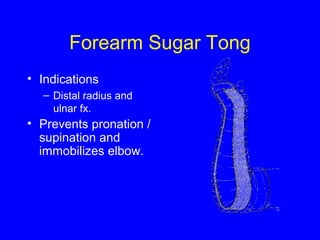
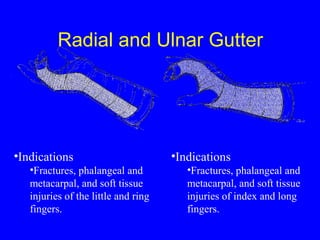
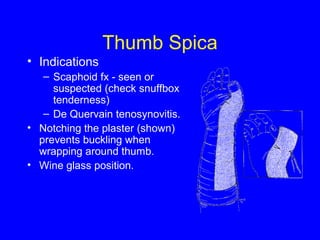
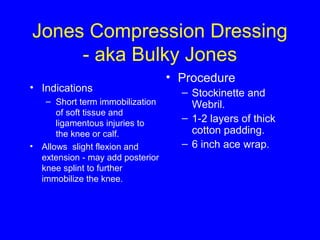
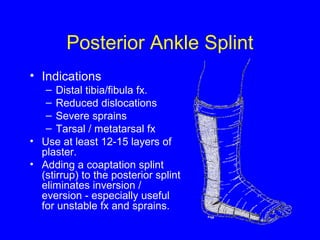
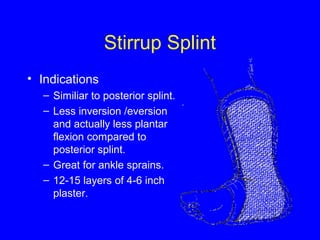
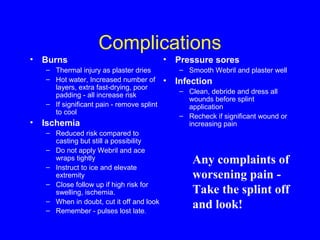
This document provides information on orthopedic injuries and immobilization. It discusses evaluating neurovascular status and injury mechanism upon presentation. Reduction and immobilization with splinting or casting is recommended for fractures and dislocations. Specific techniques are described for reducing various injuries like shoulder dislocations. Common fracture types and locations are outlined. Detailed instructions are provided on splint construction and types for different body parts like the forearm, wrist, fingers and ankle. Complications of splinting like burns and ischemia are also addressed.