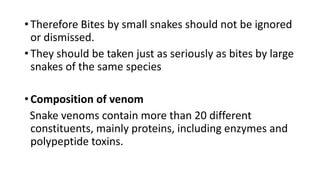
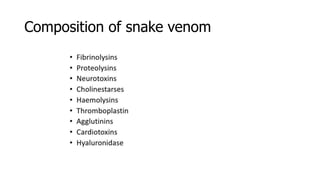
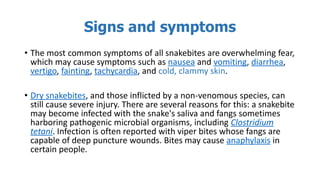
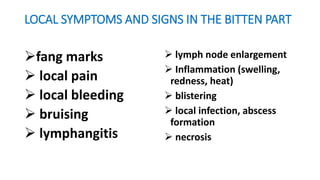
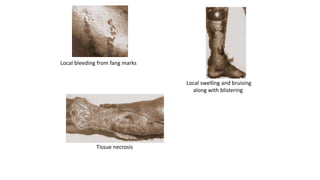
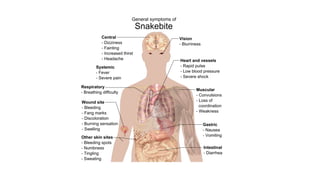
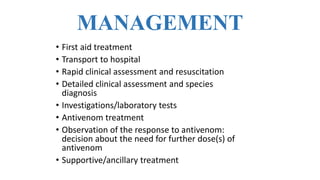
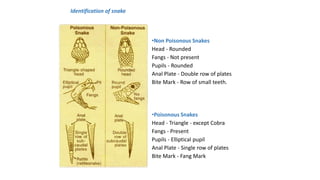
Animal bites, particularly from snakes and domestic animals like dogs, pose significant health risks globally, with children being the most affected demographic. Timely medical intervention is crucial for managing envenomation from snake bites and preventing complications, while educational measures can help reduce the incidence of such injuries. Management involves first aid, accurate diagnosis, and the administration of antivenom along with supportive care to address various clinical signs and symptoms.


![EPIDEMIOLOGY
• Estimate vary from 1.2 to 5.5 million snakebites, 421,000 to
2.5 million envenomings, and 20,000 to 125,000 deaths
globally.
• According to Deikumah JP et. Al (2023), In Northern Ghana,
there were an estimated 86 envenomings and 24
deaths/100,000/year caused mainly by Echis ocellatus [5]
while other studies in the Brong-Ahafo Region of Ghana
found snakebite incidence of 92/100,000.](https://image.slidesharecdn.com/animalbitespresentation-240427133810-9c33c8b1/85/ANIMAL-BITES-PRESENTATION-2024-by-P-pptx-8-320.jpg)