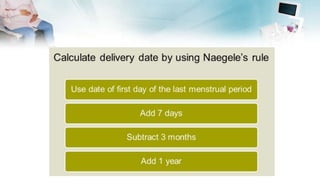
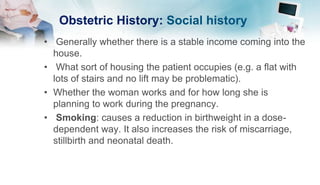
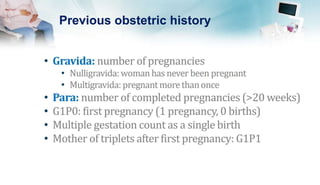
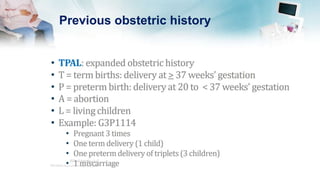
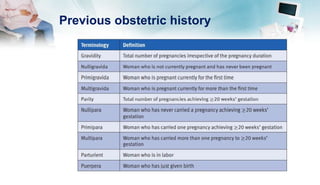
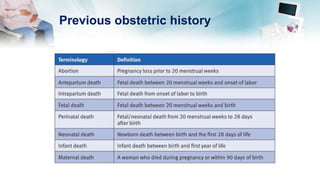
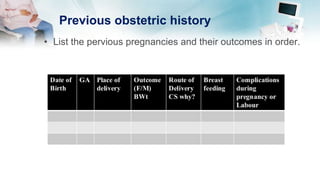
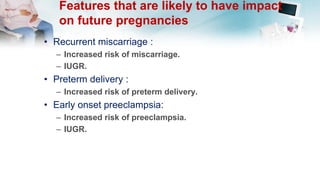
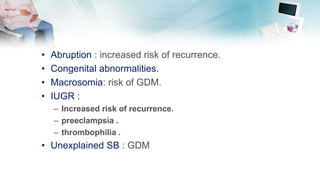
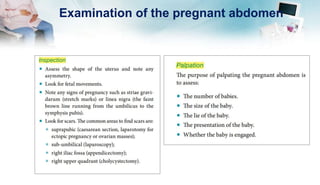
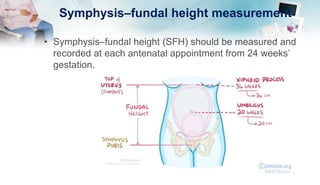
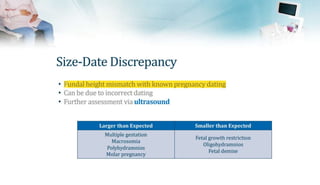
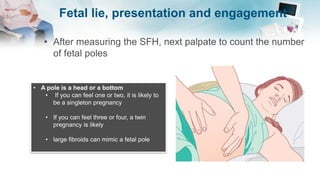
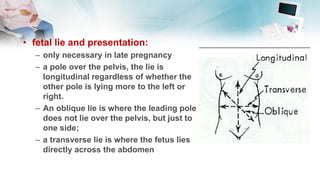
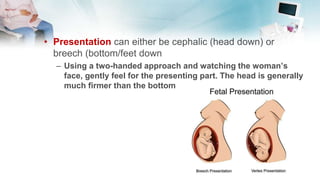
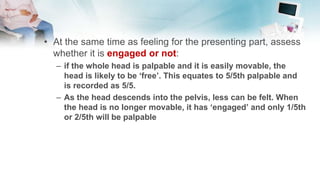
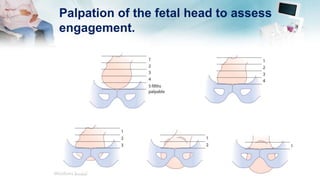
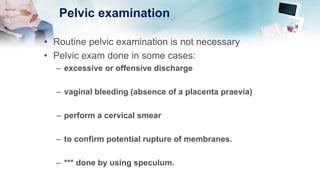
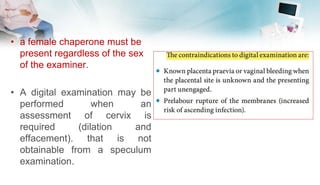
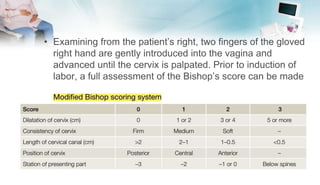
The document outlines the essential components of taking an obstetric history and conducting an obstetric examination, emphasizing the tailored approach necessary throughout different stages of pregnancy. Key areas covered include demographic details, medical and social histories, previous obstetric experiences, and vital examinations like blood pressure and fetal assessments. It stresses the importance of sensitivity and adherence to infection control during examinations, as well as recognizing risk factors associated with maternal and fetal health.