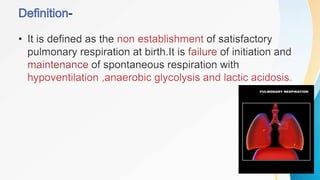
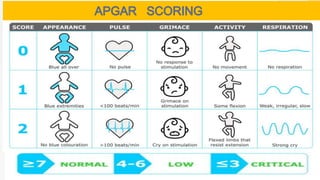
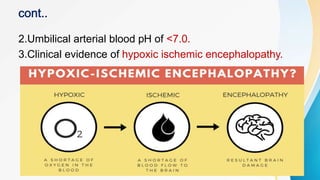
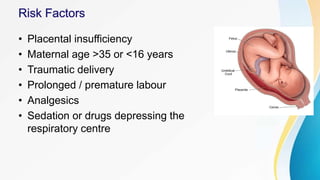
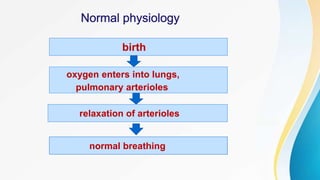
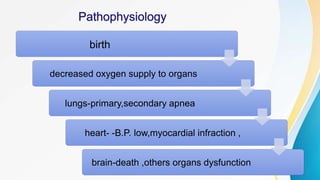
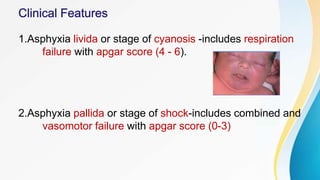
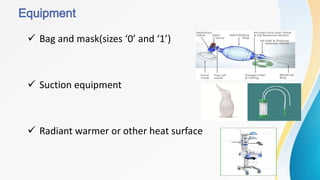
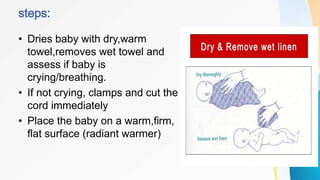
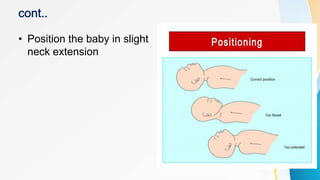
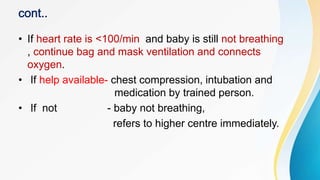
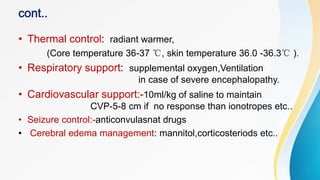
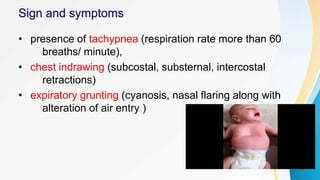
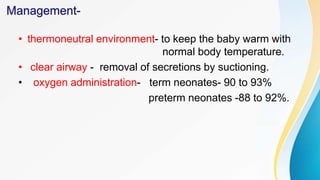
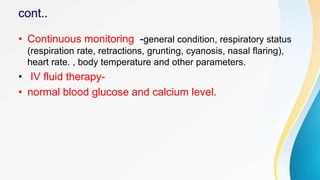
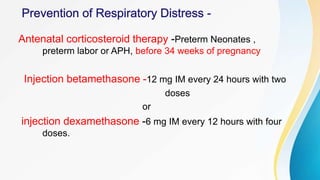
Birth asphyxia and respiratory distress are common conditions in newborns that can lead to neonatal death if not properly managed. Birth asphyxia is caused by a lack of oxygen during delivery and is diagnosed using the Apgar score and umbilical cord blood pH. Respiratory distress in newborns has pulmonary causes like respiratory distress syndrome or nonpulmonary causes like perinatal asphyxia. Management of both conditions involves providing oxygen, monitoring vital signs, treating infections, and supporting respiratory and cardiovascular functions. Timely identification and treatment can improve prognosis.