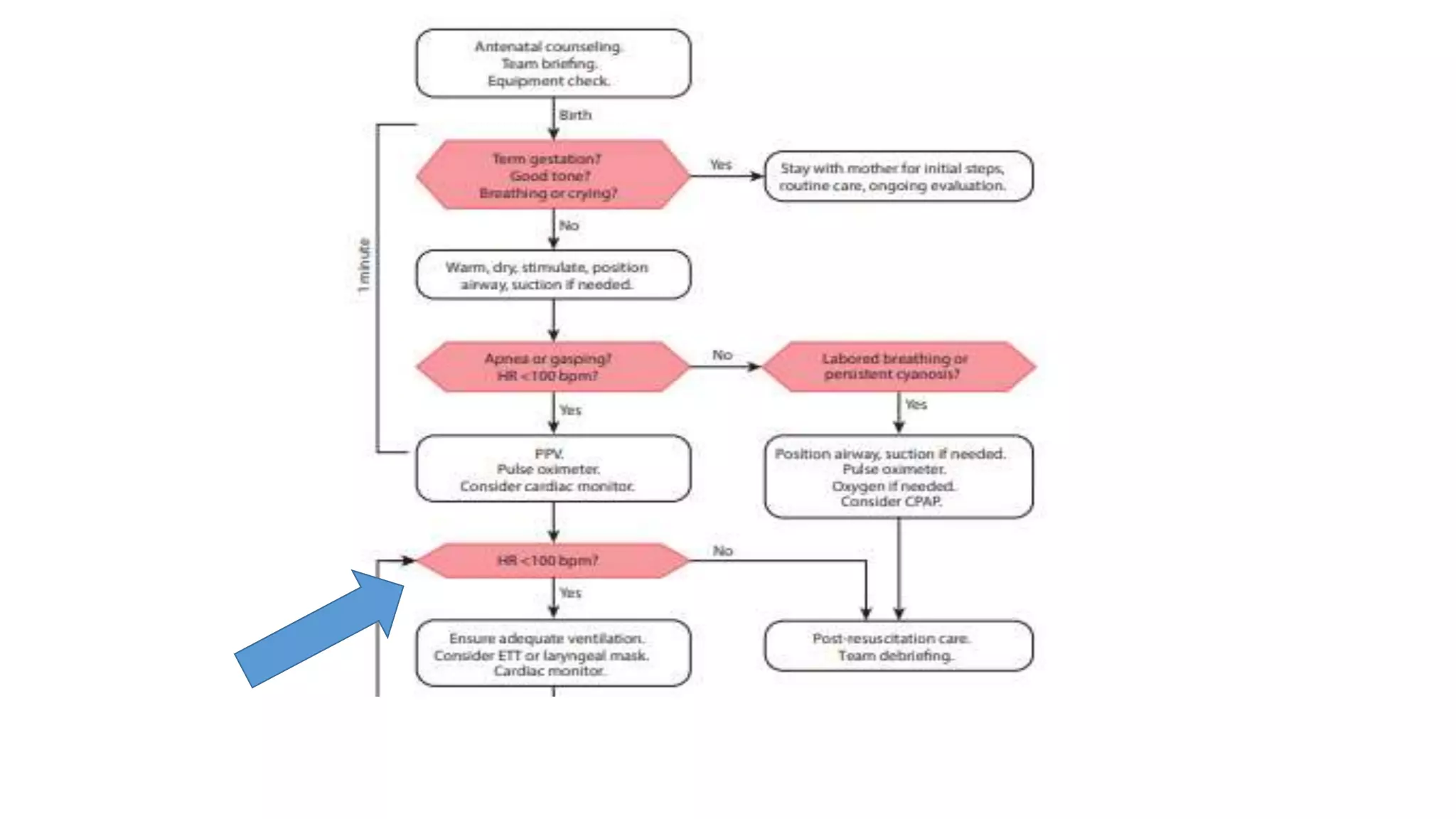
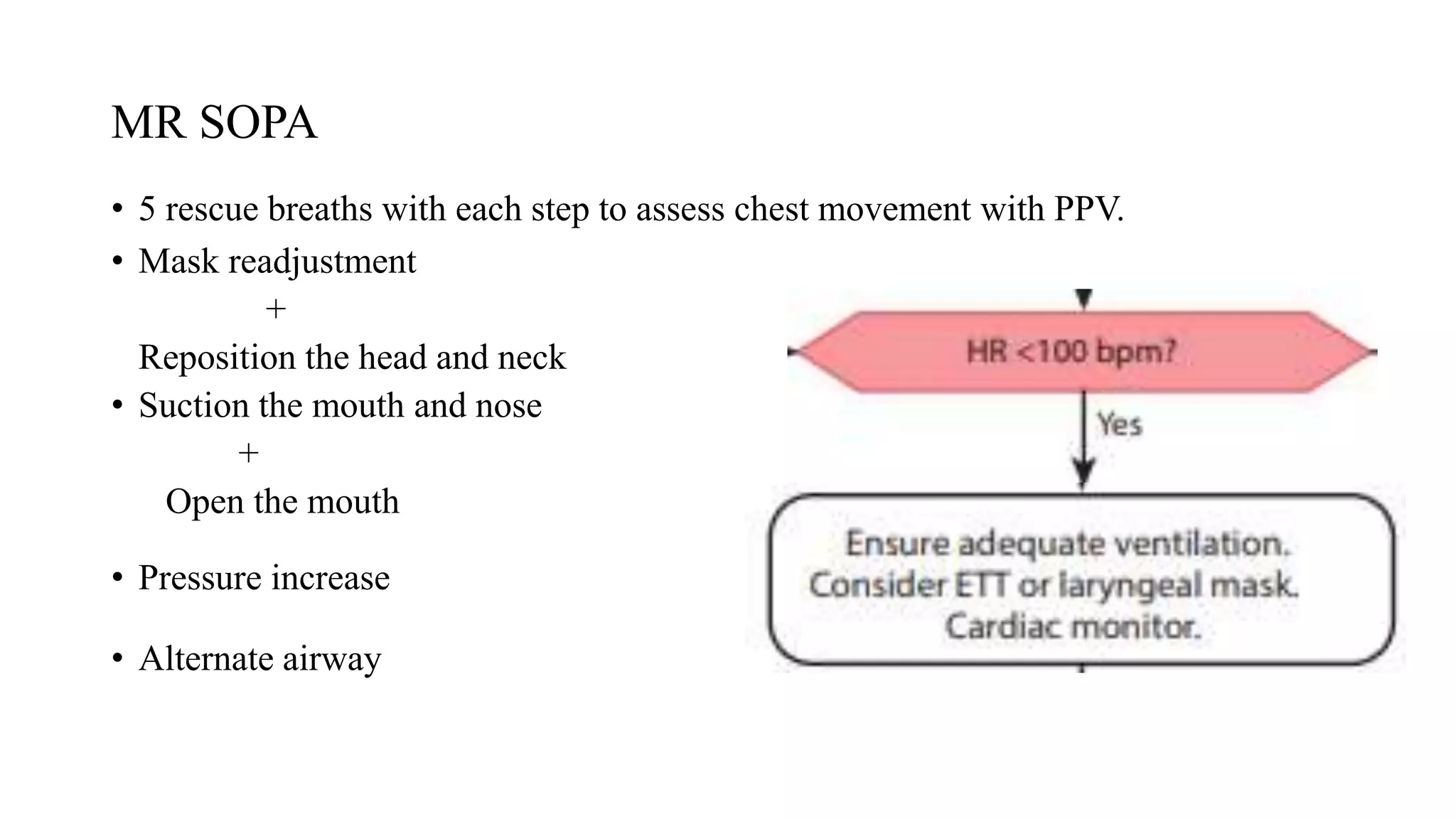
This document summarizes the NALS algorithm for neonatal resuscitation presented by Dr. Kiran Dyavanagoudar. The algorithm is divided into 5 blocks beginning with birth and initial assessment. It describes the steps of positive pressure ventilation, indications for endotracheal intubation and chest compressions, and medications used in neonatal resuscitation such as epinephrine. Anticipation and preparation by the resuscitation team is important. Ventilation of the newborn's lungs is the most important step, and an increase in heart rate indicates effective resuscitation.