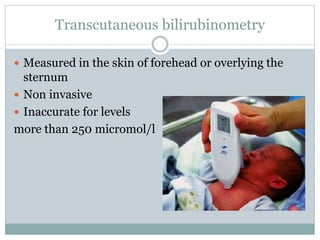
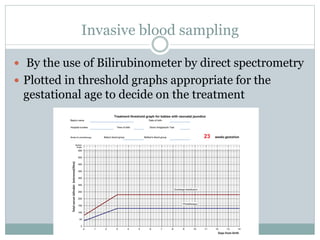
This document provides an overview of neonatal jaundice, including its definition, clinical features, causes, complications, investigations, and management. Some key points include:
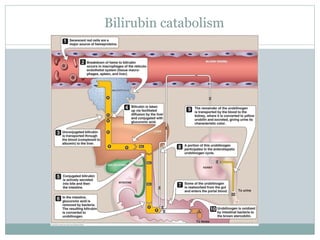
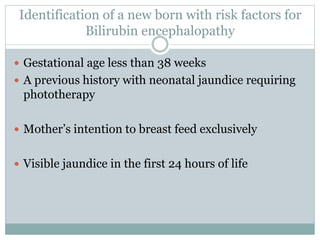
- Jaundice is a common condition in newborns caused by accumulation of bilirubin in the skin.
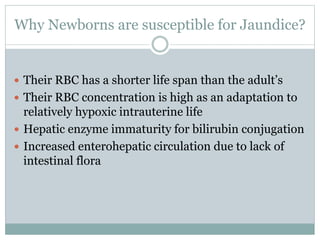
- It results from the normal breakdown of red blood cells in combination with the immature liver's ability to process bilirubin in newborns.
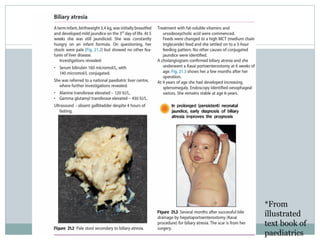
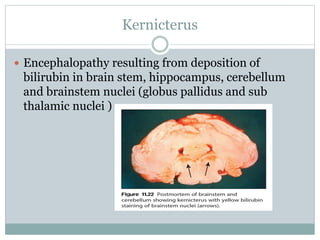
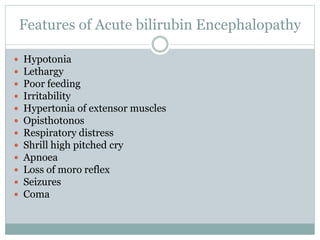
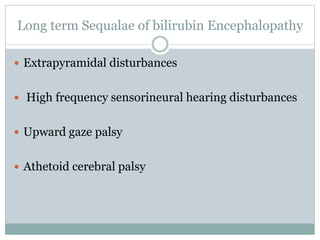
- If left untreated, extremely high bilirubin levels can cause brain damage (kernicterus).
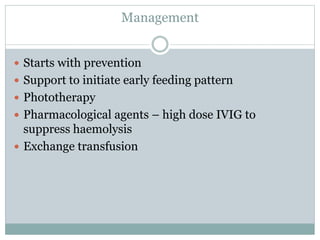
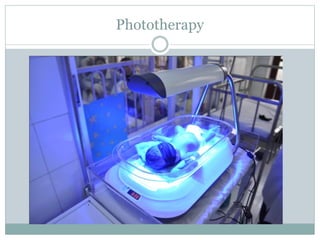
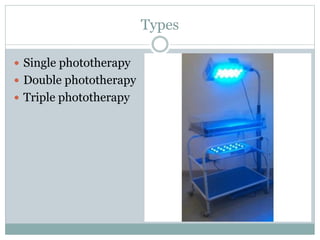
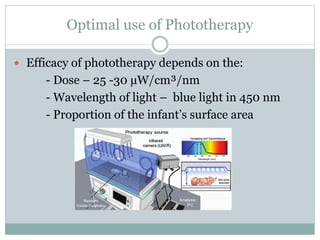
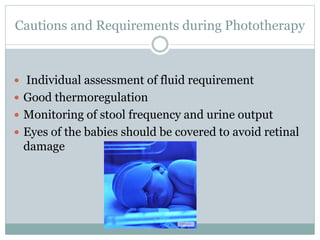
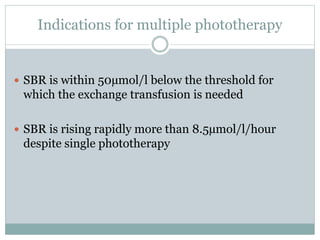
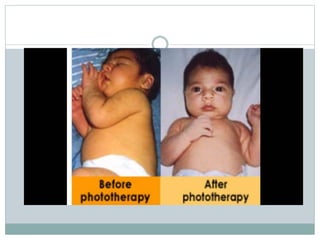
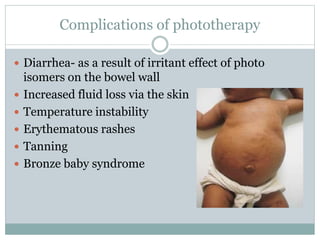
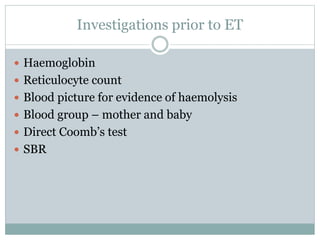
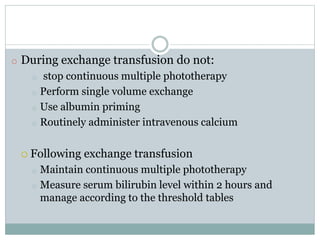
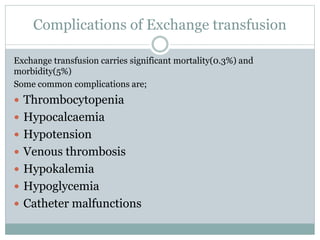
- Treatment involves phototherapy or exchange transfusions in severe cases to lower bilirubin levels.
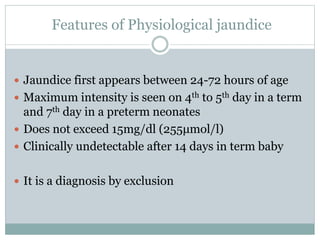
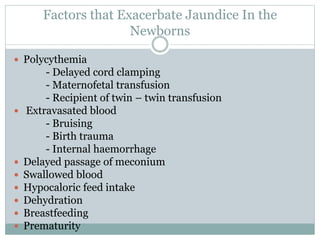
- Causes of jaundice include physiological causes or